Fatigue Units: A Conversation with BDG Research Director Dr. Mike Sonne
Last week, Baseball Development Group had it’s preliminary 2019 ‘Research Meeting’ to discuss our upcoming plans, projects, and talk shop about what we want to accomplish in the next twelve months (there are some cool things that we can get into that later on in this blog).
At the end of the meeting, we decided that it would probably be a good idea to have a conversation with our Research Director, Dr. Mike Sonne (@drmikesonne), to go over his background, what he’s looking into, and our future endeavours at BDG. Here’s a copy of our conversation – buffed up afterwards with some editing.

Dr. Mike Sonne has a PhD in biomechanics from McMaster University in Hamilton, where he studied muscle fatigue and how it influences performance. In the last few years he’s gotten very involved in baseball; having been a recurring guest to Pitch Talks and the Fan 590 Sportsnet, writing for The Athletic and his blog, and now working as the Director of Research with us!
[Steve] Alright Mike, time to get down to business and show off that brain of yours. Can you maybe elaborate a little bit on your PhD thesis, your interest in baseball and why you publicly boo the PA announcement of pitch clocks at baseball games? (he actually did that with me)
[Mike] Sure! I started my degree in Human Kinetics, thinking I’d full well get into the field of Athletic Therapy. I had been involved in AT as a student trainer, all throughout high school. By the end of my undergrad, I took a bit of a different turn, and got into the world of ergonomics – and primarily, coming up with new ways to evaluate the risks in how people work.
In my PhD work, I studied muscle fatigue. (You can find Mike’s research here) The goal of this work, was to come up with a model that could be used to evaluate jobs, and determine which ones would cause people to fatigue more. So, I did a bunch of studies using different techniques to evaluate fatigue. We ended up modifying an existing model, and integrating the physiological principles of motor units, to help better predict fatigue. The final product was a model that required a series of muscle demands, and specified rest breaks, and we could get an idea of how much fatigue a muscle had incurred.
I’ve always been a big baseball fan. I pitched a bit in the earlier part of high school, but my mid 50’s cheese didn’t really hack it. My family have been massive Blue Jays fans for my whole life. As I got further into the fatigue research, I found some interesting articles that evaluated the muscle demands of pitching, and felt I could use those to assess fatigue – using that same fatigue model – in pitchers.
A common issue that we have in ergonomics, is when engineers add jobs to the assembly line, thus decreasing the amount of rest workers have while doing their job. The demands themselves, are acceptable still – they don’t exceed the strength demands of the workers, but now they don’t have enough time to recover. Over the course of an 8 hour day, the fatigue levels increase, and the risk of injury increases.
[Steve]: Logically this makes a lot of sense. You’re asking pitchers to complete the same amount of work in a smaller time period. But then again, this line of thought can escape baseball in even the most ritualistic tasks. How many coaches use a stopwatch to ensure appropriate rest intervals in between pitches in a bullpen? Or progressively tweak their work:rest ratios throughout the off-season? What about taking all those hacks in a short amount of time during batting practice? These are things that we think about all the time.
[Mike] Well, in the first example – how many times are coaches getting on their pitchers to tell them – ok, now you need to throw again… RIGHT NOW!!! In ergonomics, we commonly rely on the field of psychophysics – which is, if we train someone well enough in a task, we can rely on their inner physiological, psychological, and biomechanical feedback to say “yes, I have recovered enough to perform another effort”, or “this is the maximum amount of force I could perform in a given amount of time”. The same thing goes for pitchers – how many pitches have you thrown in your life? I think it’s safe to say, by the time someone makes it to the MLB, their body is pretty in tune with what it can, or can’t do, and to force them out of their natural pace that they have self selected – that’s counter productive to player health and well-being.
[Steve] So FU’s take into consideration the number of pitches per inning, the pace at which they’re thrown, the number of days rest in between outings, and the velocity of the pitcher. I remember when you and I first talked about this, years ago now, I brought up the challenge of trying to customize this to a player’s previous throwing history.
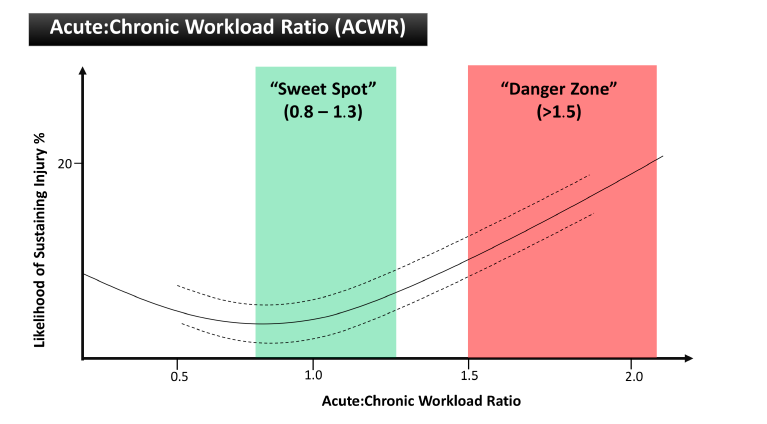
[Mike] Using FUs alongside your traditional metrics, is a great way to compare workloads between your players. For example, the Josh Hader example. Let’s say you have two pitchers going into your team’s Tournament, and both have thrown the same number of innings – though one has been appearing on back to back days more frequently. Despite similarities in workload from an innings and pitches perspective, you can see which pitcher has had a higher workload. The same works for checking to see how efficient a pitcher is. Perhaps two pitchers have thrown 30 innings, but one has a 15% higher Fatigue Unit workload than the other – this pitcher needs to be come more effective in the number of pitches they throw per inning to reduce their own workload.
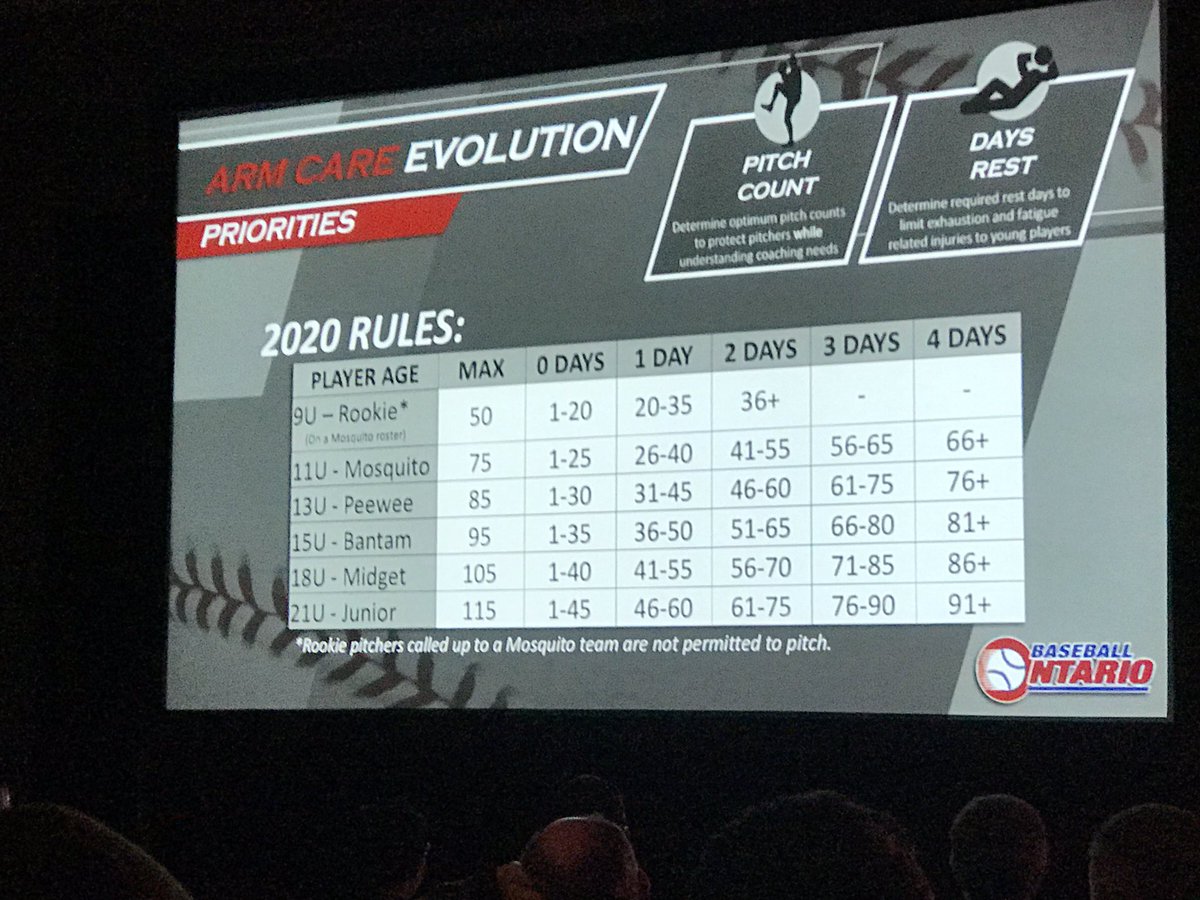
The Baseball Ontario Pitch Guidelines are going to change in 2020 to be much better aligned with contemporary concepts regarding workload management. Dr. Mike Sonne is on the advisory board for the committee addressing these changes.
[Mike] When it comes to the arm care guidelines with Baseball Ontario, we’re going to use all of the available scientific literature to propose some new ideas, but then rely on the expertise of coaches and trainers to help us achieve successful and reasonable implementation. These things only work if everyone is on board.
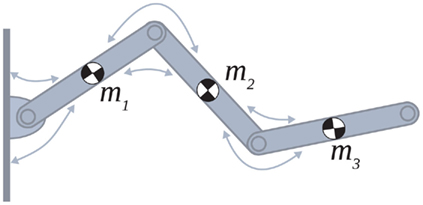
Co-contraction provides stability at a joint, but with too much of it comes rigidity in movement.
The theory that I have, is with pitching exercises like weighted baseballs, and throwing with maximum intent. To achieve absolute maximum velocity and movement speed, you’re going to have to turn off some of those safeguards – joint rotational stiffness has to decrease. While we’ve seen some studies citing that weighted baseballs don’t increase the stress on the arm, the amount of co-contraction really isn’t taken into consideration. Dr. James Buffi – subject of Jeff Passan’s book “The Arm”, and current Dodgers employee, created a model that would look at the relative contributions of muscle activity to the stress on the UCL. What his model would show in this phenomena, is that overall stress on the elbow isn’t changed when throwing a weighted baseball, but the amount of force transmitted directly to the UCL would be increased.
[Steve] He’s a hard working guy with a bright future for sure. Looking forward to seeing the final touches on his study.
[Mike] BDG has always focused on making sure the human body is capable of performing the tasks we ask of it, and then finding the best ways to recover from those types of activities. Our first official research studies are going to be focused on this exact topics.
We’ll also be working with Dr. Nick La Delfa and Dr. Adam Murphy at the University of Ontario Institute of Technology to look at the basic physiological and biomechanical factors surrounding pitching performance. Lots of videos get posted on social media talking about whether or not a pitcher should lift, or how much they should lift. Should they be focused on flexibility or strength? We’ll be capturing those factors, as well as other factors like co-contraction, on performance metrics captured by the Rapsodo system. It’s been a long time coming, but it’s time you got to meet Reviewer #2, Steve!
Your blog stands out in a sea of generic and formulaic content Your unique voice and perspective are what keep me coming back for more
Asking questions are truly fastidious thing if you are not understanding
anything completely, except this article provides nice understanding yet.
Tu salud no tiene precio, y si es con descuento en Laboratorios Chopo, ¡mejor aún!
Looking forward to your next post. Keep up the good work!
OK9 THỂ THAO XANH CHÍN – LINK OK9.COM OK9AA UPDATE T6/2025 ĐĂNG KÝ +99K
OK9 – TRANG CHỦ NHÀ CÁI OK9.COM OK9AA – LINK TẢI APP OK9 MỚI NHẤT 2025
Lương Sơn TV là kênh trực tiếp bóng đá hàng đầu tại Việt Nam, nơi hội tụ mọi trận cầu đỉnh cao mỗi ngày với chất lượng hình ảnh Full HD, âm thanh sống động và hoàn toàn miễn phí. Không cần tài khoản, không quảng cáo gây phiền, chỉ cần truy cập là bạn có thể đắm chìm trong không khí sôi động của những giải đấu lớn như Ngoại hạng Anh, Champions League, La Liga, Bundesliga hay V-League. Hãy cùng khám phá vì sao Luong Son TV ngày càng được yêu thích trong cộng đồng yêu bóng đá trực tuyến.
LuongSon TV là kênh trực tiếp bóng đá full HD hàng đầu VIỆT NAM, không chỉ thu hút khán giả trẻ mà còn mở rộng sức hút đến mọi lứa tuổi, kết nối cộng đồng yêu môn thể thao vua. LuongSon trực tiếp bóng đá hàng loạt trận cầu đỉnh cao cùng thông tin chi tiết như Tin tức, Bảng xếp hạng, Soi kèo, và Highlight đặc sắc, khẳng định vị thế là lựa chọn hàng đầu của người hâm mộ bóng đá. Nếu bạn yêu môn thể thao vua, nền tảng này là nơi mang đến trải nghiệm bóng đá trực tuyến tuyệt vời, khiến bạn không thể bỏ lỡ!
LuongSon TV là kênh trực tiếp bóng đá full HD uy tín, chất lượng cao, nơi quy tụ hàng triệu người hâm mộ túc cầu Việt Nam mỗi ngày. Với giao diện mượt mà, không quảng cáo khó chịu, tốc độ tải nhanh và chất lượng Full HD, nền tảng này đang dần trở thành lựa chọn hàng đầu cho những ai đam mê bóng đá. Dù bạn yêu Ngoại hạng Anh, Champions League hay các trận V-League, LuongSon đều có đầy đủ link trực tiếp và thông tin đi kèm.
Trong kỷ nguyên số, việc thưởng thức bóng đá mọi lúc, mọi nơi đã trở thành nhu cầu không thể thiếu với hàng triệu người hâm mộ. LuongSon TV ra đời như một nền tảng hoàn hảo, đáp ứng trọn vẹn tiêu chí: miễn phí, tiện lợi và chất lượng. Tại đây, người xem có thể tận hưởng không khí sôi động của những trận cầu đỉnh cao chỉ với một cú click.
LuongSon TV chính là lựa chọn lý tưởng, đáp ứng mọi nhu cầu của người hâm mộ từ hình ảnh sắc nét, đường truyền mượt mà đến lịch thi đấu cập nhật liên tục. Với vị thế ngày càng vững chắc, LuongSonTV đang trở thành cái tên quen thuộc với cộng đồng yêu bóng đá tại Việt Nam và khu vực.
ABC8 là địa chỉ cá cược online quen thuộc của nhiều tay chơi chuyên nghiệp hiện nay. Nhà cái cung cấp hàng loạt tựa game cực hấp dẫn cùng dịch vụ chỉn chu đi kèm. Đến với sân chơi, thành viên chắc chắn sẽ có những trải nghiệm, những phút giây giải trí ấn tượng và hài lòng.
ABC8 là nhà cái trực tuyến hàng đầu nổi bật với sự uy tín và chất lượng dịch vụ vượt trội. Được cấp phép hoạt động bởi các tổ chức quản lý uy tín tại Philippines, ABC 8 cung cấp đa dạng sản phẩm cá cược như thể thao, casino, bắn cá, đá gà, xổ số. Nhà cái luôn chú trọng đến sự minh bạch, công bằng cùng với hệ thống bảo mật tiên tiến, đảm bảo trải nghiệm an toàn và tiện lợi cho người chơi.
88CLB là điểm đến của những tín đồ yêu thích sự công bằng, minh bạch và trải nghiệm giải trí đổi thưởng đỉnh cao. Với công nghệ hiện đại, giao diện thân thiện, bảo mật tuyệt đối cùng kho game đồ sộ nền tảng đã khẳng định vị thế tiên phong trong làng cá cược khu vực.
Lương Sơn TV đã và đang khẳng định vị thế là một trong những trang web xem bóng đá trực tuyến miễn phí được tin tưởng và yêu thích nhất tại Việt Nam. Với giao diện thân thiện, tốc độ tải mượt mà và nguồn phát ổn định, LuongSon TV mang đến trải nghiệm xem bóng đá chất lượng cao, phù hợp với mọi đối tượng người dùng – từ fan cuồng nhiệt đến những người chỉ theo dõi vì đam mê.
Với xu hướng người dùng chuyển sang theo dõi bóng đá qua nền tảng trực tuyến ngày càng tăng cao, LuongSon TV đã nhanh chóng nắm bắt và xây dựng một kênh trực tiếp bóng đá để phục vụ trọn vẹn nhu cầu xem bóng đá mỗi ngày. Không chỉ đơn thuần là kênh phát sóng, LuongSon còn là nơi kết nối cộng đồng fan túc cầu, cập nhật tin tức, highlight, lịch thi đấu, soi kèo và nhiều tiện ích giá trị khác.
LuongSon tv định hướng trở thành nền tảng xem bóng đá trực tuyến hàng đầu Đông Nam Á, cung cấp trải nghiệm chuẩn quốc tế cho người Việt. Không chỉ dừng lại ở phát sóng, LuongSonTV còn hướng đến việc xây dựng cộng đồng bóng đá số hóa sôi động.
LuongSon tv định hướng trở thành nền tảng xem bóng đá trực tuyến hàng đầu Đông Nam Á, cung cấp trải nghiệm chuẩn quốc tế cho người Việt. Không chỉ dừng lại ở phát sóng, LuongSonTV còn hướng đến việc xây dựng cộng đồng bóng đá số hóa sôi động.
LuongSon TV không chỉ đơn thuần là một website phát sóng tructiepbongda, mà là cầu nối giúp hàng triệu người hâm mộ bóng đá tiếp cận các giải đấu lớn như Ngoại hạng Anh, Cúp C1, La Liga, Bundesliga, Serie A… Với hệ thống máy chủ tối ưu, nền tảng này mang lại trải nghiệm xem bóng đá không giật, không lag, điều mà ít kênh miễn phí nào có thể duy trì ổn định như vậy.
HB88 thường xuyên có các chương trình khuyến mãi, ưu đãi hấp dẫn dành cho người chơi. Từ các chương trình chào mừng dành cho tân thủ, đến các chương trình ưu đãi nạp tiền, hoàn trả cược,…
Bundesliga thay đổi chóng mặt mỗi tuần, fan Bayern không thể bỏ lỡ. Theo dõi toàn bộ bảng điểm, thứ hạng và tỷ số. Tất cả có tại bxh Bundesliga chính xác từng vòng.
Real, Barca, Atletico… đá trận nào, giờ nào đều có đủ. Lịch La Liga được cập nhật tự động sau từng vòng. Click vào lịch thi đấu La Liga để theo dõi.
LuongSon TV là nền tảng phát sóng bóng đá trực tuyến được quan tâm nhất hiện nay, mang đến cho người hâm mộ những trận cầu hấp dẫn từ khắp nơi trên thế giới. Với cam kết xem miễn phí và chất lượng hình ảnh vượt trội, LuongSon tạo nên không gian giải trí sôi động, nơi mọi người có thể cùng nhau thưởng thức bóng đá, bình luận, và chia sẻ ý kiến trong cộng đồng yêu thể thao. Đây chính là điểm đến lý tưởng cho những người đam mê trái bóng tròn!
Pretty! This was an incredibly wonderful post. Many thanks for providing this info.
Ra đời tại Châu Âu và mở rộng sang thị trường Châu Á từ năm 2014, 98WIN đã xây dựng được vị thế vững chắc trong ngành giải trí trực tuyến. Nhà cái này nổi bật nhờ hệ thống bảo mật tiên tiến, dịch vụ chất lượng cùng hàng loạt tựa game hấp dẫn, mang đến trải nghiệm đỉnh cao cho người dùng.
Trực tiếp bóng đá LuongSon TV được thành lập với tâm huyết từ những người yêu bóng đá, hiểu rõ nhu cầu cập nhật thông tin của người hâm mộ Việt Nam.
OK9 không chỉ là nhà cái online uy tín, mà còn là nơi quy tụ cộng đồng cược thủ chuyên nghiệp. Giao diện hỗ trợ tiếng Việt, app cược tối ưu cho mobile, và chương trình thưởng VIP hấp dẫn giúp OK9 luôn giữ vững top đầu thị trường cá cược trực tuyến.
OK9 – Đẳng cấp nhà cái quốc tế với hơn 1 triệu thành viên toàn cầu. Được cấp phép bởi tổ chức uy tín và bảo mật theo chuẩn châu Âu, OK9.COM mang đến trải nghiệm cược thể thao, casino online và game bài đổi thưởng an toàn – tiện lợi – hấp dẫn mỗi ngày.
23WIN là một trong những nhà cái cá cược trực tuyến uy tín được nhiều người chơi tại Việt Nam tin tưởng nhờ sản phẩm giải trí đa dạng, dịch vụ chất lượng cao và đặc biệt là hệ thống chương trình khuyến mãi phong phú, hấp dẫn. Giao diện tại 23win.com được thiết kế hiện đại, dễ sử dụng cùng dịch vụ chăm sóc khách hàng chuyên nghiệp, tận tâm luôn sẵn sàng giải đáp thắc mắc và xử lý yêu cầu của khách hàng 24/7.
Bet88.com was established in 2007 and operates legally under the license of PAGCOR – the Philippine Amusement and Gaming Corporation. This license ensures that all of Bet88’s operations are transparent, fair, and fully compliant with international standards.
Owned by Cube Limited, a well-known name in the online entertainment industry, Bet88 odds provide players with complete peace of mind — delivering a secure, trustworthy, and world-class betting experience.
Không cần tìm xa, OK9.COM là điểm chơi cá cược đáng tin cậy với hàng loạt tiện ích: đăng ký dễ dàng, link vào OK9 không bị chặn, code thưởng mỗi ngày, cùng hàng trăm trò chơi casino và thể thao với tỷ lệ kèo đỉnh cao.
XX88 là nền tảng giải trí tiên phong tại Việt Nam, chuyên cung cấp đa dạng trò chơi đổi thưởng hấp dẫn: từ casino trực tuyến, slot, bắn cá, đến xổ số và thể thao.
BET88 is a premier entertainment brand offering a comprehensive betting ecosystem with over 1,000 games, serving more than 1 million customers across Southeast Asia. Fully licensed by PAGCOR, BET88 guarantees an explosive and secure betting experience.
What sets BET88 apart is its lightning-fast withdrawals, averaging just 3 minutes, and a verified RTP (Return to Player) rate of up to 97% by iTech Labs — giving players greater confidence and fairness in every session.
007win is a trusted bookmaker in Vietnam, known for its user-friendly interface, professional customer service, and a wide selection of betting games. Key advantages include high-level security, fast and seamless transactions, attractive promotions, and 24/7 player support, all designed to deliver the best possible experience for every user.
KUBET11 is a leading online gaming platform that offers a safe, transparent, and premium betting experience. With a modern interface, lightning-fast processing speed, and advanced security systems, KUBET11 is committed to providing players with the highest quality entertainment environment available.
ABC88 is recognized as one of the most professional and reputable bookmakers on the market today. With a range of outstanding advantages, players can enjoy a variety of exciting games, take part in massive promotions, and win big rewards.
To learn more about what makes ABC88 a top choice for bettors, keep reading the detailed information shared below.
As the online betting industry continues to grow rapidly, players must be more cautious in choosing a reliable and trustworthy platform. Among countless options on the market, 9BET stands out as a premium bookmaker — not only attracting a large player base but also solidifying its strong position in Southeast Asia and beyond.
With a diverse range of entertainment products, optimized services, and exciting promotions, 9BET continues to lead the way in shaping the future of online betting.
HUBET is a trusted online betting platform offering a wide range of entertainment services, including sports betting, live casino, card games, lottery, and slot games. Fully licensed and legally operated, HUBET is committed to providing a transparent, secure, and fair environment for all players.
With a user-friendly interface, 24/7 customer support, and attractive promotions, HUBET has become a reliable choice for thousands of users. Continuously evolving, HUBET adds new features and improves its system to deliver the highest level of satisfaction and an enhanced betting experience.
Luck8 is a leading and trusted online betting platform, offering a top-tier entertainment experience with a wide range of products including sports betting, live casino, lottery, fish shooting, jackpot slots, and card games.
With a user-friendly interface, high-level security, and 24/7 customer support, Luck8 is committed to providing a safe, fair, and reliable betting environment for all users.
88vv.com is currently rated as one of the most reputable online entertainment platforms, bringing together everything modern players look for — from a user-friendly interface and ultra-fast deposits and withdrawals to a diverse ecosystem that includes online sports betting, jackpot slot games, live casino, fish shooting, and much more.
What truly sets 88vv apart is its strong focus on user experience, data security, and transparent transactions.
Visit the official homepage of 88vv today to discover why it stands out as a trusted choice among countless betting platforms.
789win proudly stands as one of Asia’s leading online betting platforms, bringing together a global community of over 8 million members who share a passion for sports, casino games, and reward-based gaming.
Legally licensed by Curacao eGaming, 789WIN is committed to providing a safe, transparent, and highly secure betting environment, backed by cutting-edge 256-bit SSL encryption technology.
With a comprehensive gaming ecosystem, 789win delivers everything players need for a top-tier entertainment experience — all in one trusted platform.
Vin88 proudly stands as one of Asia’s most reputable and high-quality online betting platforms, specializing in a wide range of trusted and engaging services. These include live casino, sports betting, lottery, card games, jackpot slots, and many other exciting options.
Highly rated for both credibility and service quality, Vin88 has successfully attracted a large and growing player base across the region — making it a top destination for online entertainment and betting.
789win là một nhà cái cá cược uy tín với đa dạng trò chơi từ casino, thể thao đến các trò chơi slot hấp dẫn. Sân chơi thu hút người chơi bởi giao diện dễ sử dụng, các chương trình khuyến mãi hấp dẫn.
Vipwin is a top-tier and highly trusted betting platform, offering a wide variety of games to suit every type of player. With hundreds of exciting games and a rich selection of bonuses and promotions, Vipwin ensures that every member enjoys both thrilling entertainment and rewarding opportunities.
With our breadth of knowledge and experience there’s no security requirement we
can’t meet.
8XBET – The Ultimate Entertainment Playground
Experience top-tier betting with 8XBET, a trusted platform known for its security, game variety, and reliability. With fast support and flexible payment options, 8XBET is committed to delivering a premium-quality service for players across Vietnam.
Luongsontv mang đến trải nghiệm bóng đá trực tuyến chất lượng Full HD, phát sóng miễn phí các giải đấu lớn nhỏ trên toàn thế giới như Ngoại hạng Anh, La Liga, Bundesliga, Series A và Champions League, V-League giúp bạn không bỏ lỡ bất kỳ trận đấu nào.
8XBET is more than just an online betting platform — it’s a trusted hub where transparency, convenience, and dedicated support come together. With a user-friendly interface, competitive odds, and 24/7 customer service, 8XBET continues to earn the trust of both seasoned players and newcomers alike.
👉 If you’re looking for a reliable, easy-to-use, and fast-paying platform, visit the official 8XBET homepage now to start your journey.
Sign up today and unlock a series of exclusive promotions specially designed for new members!
WW88 is not just an online betting site with a modern interface — it also stands out for its fast transactions, wide variety of games, and transparent promotions. Whether you’re a newcomer or a seasoned player, WW88 remains a trusted choice for both entertainment and boosting your chances of winning every day.
This information is invaluable. Where can I find out more?
UU88 is a trusted platform that provides fast and accurate odds from top-tier tournaments, updated daily to help players place bets with confidence and increase their chances of winning.
Beyond sports betting, UU88 also features a rich selection of entertainment options, including casino games, poker, fish shooting, cockfighting, and lottery — offering a complete and engaging experience for every type of player.
Its like you learn my mind! You appear to grasp a lot approximately
this, such as you wrote the guide in it or something.
I feel that you could do with some % to force the message home a bit, but other
than that, that is fantastic blog. A great read.
I’ll certainly be back.
789F – 789F.events nhanh chóng theo kịp xu hướng giải trí trực tuyến, từng bước khẳng định vị thế trong thị trường cạnh tranh khốc liệt.
hello!,I like your writing very much! share we communicate extra about your post on AOL?
I need an expert on this space to solve my problem.
May be that’s you! Looking ahead to see you.
GK88 proudly launches the “Rookie Tournament 2025” – a competition designed exclusively for newcomers to the gaming and betting community. No experience required, no large capital needed — new players will compete in a dedicated bracket with easy-to-understand rules and attractive starting prizes.
With a tiered ranking system, you can compete confidently without facing seasoned pros. This is more than just a tournament — it’s your first step into the world of slots, baccarat, and fish shooting, all within a fair and transparent environment.
GK88 guarantees 24/7 support and is offering exclusive bonus codes for all newly registered accounts.
GK88 proudly launches the “Rookie Tournament 2025” – a competition designed exclusively for newcomers to the gaming and betting community. No experience required, no large capital needed — new players will compete in a dedicated bracket with easy-to-understand rules and attractive starting prizes.
With a tiered ranking system, you can compete confidently without facing seasoned pros. This is more than just a tournament — it’s your first step into the world of slots, baccarat, and fish shooting, all within a fair and transparent environment.
GK88 guarantees 24/7 support and is offering exclusive bonus codes for all newly registered accounts.
Five88 is one of the leading online betting platforms in Vietnam, widely recognized for its excellence in football betting and online card games. With a strong reputation and a growing community of passionate players, Five88 has quickly become the go-to choice for betting enthusiasts nationwide.
To learn more about what makes Five88 stand out, explore the detailed information below.
32WIN không chỉ đơn thuần là một nền tảng giải trí trực tuyến, mà còn là một điểm đến lý tưởng cho những ai yêu thích sự thử thách và khám phá.
LuongSonTV – điểm đến của những trái tim yêu bóng đá đích thực. Không chỉ phát sóng miễn phí các trận cầu đỉnh cao, nền tảng này còn mang đến trải nghiệm mượt mà, không quảng cáo chen ngang, giúp người xem sống trọn từng phút giây cùng nhịp đập sân cỏ.
Bet88 is steadily establishing its reputation in the online betting industry thanks to its stable platform, user-friendly interface, and responsive customer support. With a smooth user experience and a strong emphasis on transparency, Bet88 is a reliable and long-term choice for those seeking a trustworthy online entertainment destination.
Bet88 is steadily establishing its reputation in the online betting industry thanks to its stable platform, user-friendly interface, and responsive customer support. With a smooth user experience and a strong emphasis on transparency, Bet88 is a reliable and long-term choice for those seeking a trustworthy online entertainment destination.
23win is a leading online betting platform in Southeast Asia, renowned for its outstanding reputation and diverse game offerings — from sports betting and live casino to high-stakes cockfighting — all paired with exceptionally generous promotions.
In 2025, 23win.com delivers a premium entertainment experience with a user-friendly interface, advanced security, and big winning opportunities.
Explore the article now at 23wintop.us.com to discover:
The platform’s legal status
Its extensive game library
Key advantages
And expert tips to maximize your winning potential.
What’s up, every time i used to check website posts here in the early hours in the
break of day, because i enjoy to gain knowledge of more and more.
I’m truly enjoying the design and layout of your blog.
It’s a very easy on the eyes which makes it much more enjoyable for me to come here and visit more often. Did
you hire out a designer to create your theme? Excellent work!
PJ
Theo nhiều thống kê mới nhất, VSBET hiện là một trong những nền tảng cá cược trực tuyến được yêu thích nhất tại Việt Nam. Không chỉ sở hữu lượng người chơi đông đảo, VSBET còn nổi bật nhờ các chương trình khuyến mãi hấp dẫn và tỷ lệ trả thưởng cực cao, thu hút hàng chục nghìn lượt đăng ký mới mỗi tháng.
23win is a leading online betting platform in Southeast Asia, renowned for its outstanding reputation and diverse game offerings — from sports betting and live casino to high-stakes cockfighting — all paired with exceptionally generous promotions.
In 2025, 23win.com delivers a premium entertainment experience with a user-friendly interface, advanced security, and big winning opportunities.
Explore the article now at 23wintop.us.com to discover:
The platform’s legal status
Its extensive game library
Key advantages
And expert tips to maximize your winning potential.
Hmm it looks like your blog ate my first comment (it was super long) so
I guess I’ll just sum it up what I wrote and say, I’m thoroughly enjoying your
blog. I as well am an aspiring blog writer but I’m still new to the whole thing.
Do you have any suggestions for novice blog writers?
I’d really appreciate it.
THABET – Tha Casino App has earned an irreplaceable place in the hearts of online betting enthusiasts. Unlike platforms that rely heavily on sponsorships or advertising, THABET has built its reputation through the real value and experiences it delivers to players.
This is more than just a betting platform — it’s a vibrant playground where users can explore a wide variety of exciting games and compete for prestigious golden prizes. THABET stands out for its rich content, trusted community, and rewarding gameplay that keeps players coming back for more.
32WIN offers a legally licensed online betting platform, authorized by PAGCOR and trusted by thousands of players. From sports betting and live casino to lottery games, the platform impresses with its modern interface, fast deposit and withdrawal system, and daily high-value promotions.
VSBET là nhà cái thể thao trực tuyến hàng đầu, nơi hội tụ của hàng nghìn trận đấu mỗi ngày với tỷ lệ kèo siêu cạnh tranh. Từ bóng đá, bóng rổ đến quần vợt, người chơi luôn có cơ hội bắt kèo sớm, cược nhanh và rút tiền linh hoạt. Tối ưu trải nghiệm cá cược thể thao chỉ có tại VSBET!
This web site definitely has all of the information I needed concerning this subject and didn?t know who to ask.
This info is worth everyone’s attention. How can I find out more?
Hi! I could have sworn I’ve been to your blog before but after browsing through some of the posts I realized it’s new to me. Nonetheless, I’m definitely happy I came across it and I’ll be book-marking it and checking back often!
Hi there, just became alert to your blog through Google, and found that it is really informative. I am gonna watch out for brussels. I?ll appreciate if you continue this in future. Many people will be benefited from your writing. Cheers!
Its like you learn my mind! You seem to understand a lot approximately this, like you wrote the e-book in it or something. I believe that you can do with a few percent to power the message house a little bit, however other than that, that is excellent blog. An excellent read. I will definitely be back.
I am truly delighted to glance at this web site posts which carries tons of useful facts, thanks for providing these kinds of information.
You got a very fantastic website, Sword lily I detected it through yahoo.
Là một trong những nhà cái hàng đầu tại thị trường châu Á, 58Win được vận hành bởi hệ thống công nghệ tiên tiến, bảo mật tuyệt đối và được cấp phép bởi tổ chức uy tín quốc tế. Người chơi tại 58Win hoàn toàn yên tâm về tính minh bạch, tốc độ giao dịch và chất lượng hỗ trợ khách hàng.
Casino trực tuyến – Bóng đá – Game đổi thưởng – Bắn cá – Lô đề online… tất cả đều có tại 8XBET!
Amazing postings. Thanks!
I blog often and I seriously thank you for your content. Your article has truly peaked my interest. I’m going to book mark your website and keep checking for new information about once per week. I opted in for your RSS feed too.
Good day! I could have sworn I’ve visited this web site before but after looking at a few of the posts I realized it’s new to me. Anyways, I’m definitely delighted I came across it and I’ll be book-marking it and checking back frequently!
Thank you for the auspicious writeup. It in fact was a amusement account it. Look advanced to more added agreeable from you! By the way, how can we communicate?
Thanks a lot for being my personal teacher on this niche. I actually enjoyed your own article very much and most of all cherished how you really handled the issues I regarded as being controversial. You are always quite kind to readers much like me and assist me in my lifestyle. Thank you.
Some truly interesting information, well written and loosely user friendly.
Thanks for your marvelous posting! I truly enjoyed reading it, you could be a great author. I will always bookmark your blog and may come back in the foreseeable future. I want to encourage you to definitely continue your great posts, have a nice morning!
I was reading some of your content on this site and I think this web site is really instructive! Continue putting up.
When some one searches for his necessary thing, so he/she desires to be available that in detail,
therefore that thing is maintained over here.
Hello, I enjoy reading through your article. I like to
write a little comment to support you.
Thank you for some other informative website. The place else may just I am getting that kind of info written in such an ideal way? I have a venture that I’m just now working on, and I’ve been at the glance out for such information.
I like this post, enjoyed this one regards for posting.
Hi there, just became alert to your blog through Google, and found that it is really informative. I am going to watch out for brussels. I?ll appreciate if you continue this in future. A lot of people will be benefited from your writing. Cheers!
789win – Sân chơi đỉnh cao cho mọi cược thủ, nơi hội tụ của uy tín, tốc độ và tỷ lệ kèo hấp dẫn nhất thị trường!
Now I am going to do my breakfast, once having my breakfast coming over again to read other news.
Kuwin là nền tảng cá cược trực tuyến uy tín, được cấp phép bởi chính phủ Philippines và chứng nhận bởi CEZA. Cung cấp dịch vụ đa dạng như cá cược thể thao, casino trực tuyến, và trò chơi slot, Kuwin Casino thu hút hơn 10 triệu người chơi tại Việt Nam nhờ giao diện thân thiện, dịch vụ chuyên nghiệp và nhiều ưu đãi hấp dẫn. Kuwin Direct – sự lựa chọn hàng đầu cho trải nghiệm giải trí đỉnh cao.
Sp8 là một trong những nền tảng cá cược trực tuyến hàng đầu hiện nay, được nhiều người chơi tin tưởng lựa chọn. Với giao diện hiện đại, dễ sử dụng cùng hệ thống bảo mật tiên tiến, nền tảng cam kết mang đến trải nghiệm giải trí an toàn và hấp dẫn. Tại đây, người chơi có thể tham gia cá cược thể thao, casino, game bài và nhiều trò chơi thú vị khác.
23WIN – nhà cái giải trí uy tín toàn cầu, điểm đến lý tưởng cho người chơi đam mê cá cược nhờ vào nền tảng công nghệ hiện đại, dịch vụ chuyên nghiệp và kho game đa dạng như: thể thao, casino, nổ hũ, bắn cá,… Với phương châm hoạt động “Uy tín – Minh bạch – Nhanh chóng”, 23Win.com không ngừng cải tiến hệ thống để mang đến tari nghiệm mượt mà, giao diện thân thiện và độ bảo mật an toàn cho tất cả hội viên.
FOR88 là nhà cái trực tuyến hợp pháp, được cấp phép bởi hai tổ chức uy tín hàng đầu – PAGCOR (Philippines) và Curaçao eGaming – đảm bảo tính minh bạch và an toàn tuyệt đối cho người chơi. Nền tảng được xây dựng với cơ chế bảo mật nghiêm ngặt, mang lại sự yên tâm tuyệt đối trong quá trình sử dụng dịch vụ.
YEU88 là một trong những nhà cái cá cược trực tuyến đang nổi lên mạnh mẽ tại thị trường châu Á, đặc biệt được người chơi tại Việt Nam quan tâm và lựa chọn. Với hệ thống hiện đại, được cấp phép hợp pháp từ các tổ chức quốc tế như PAGCOR, cùng giao diện thân thiện, tốc độ xử lý mượt mà, YEU88 nhanh chóng trở thành điểm đến lý tưởng cho những ai yêu thích cá cược thể thao, casino, slot game và nhiều hình thức giải trí trực tuyến khác.
Xin88 là nhà cái đổi thưởng trực tuyến hấp dẫn sở hữu hệ thống game phong phú và nền tảng cá cược đạt tiêu chuẩn quốc tế. Bạn có thể tham gia thử sức với nhiều thể loại sản phẩm và thu thưởng lớn mà vẫn an tâm. Tìm hiểu thông tin đầu để đăng ký nhận ưu đãi khủng.
N666 là cái tên quen thuộc trong cộng đồng cá cược với độ uy tín cao, minh bạch trong giao dịch và hệ thống trò chơi phong phú. Với tỷ lệ đổi thưởng hấp dẫn cùng nền tảng công nghệ hiện đại, N666 luôn là lựa chọn hàng đầu của bet thủ tại châu Á.
789F is a newly launched online betting platform, making its debut in Summer 2025 across the Asian market, with a special focus on Vietnam.
Operating under the domain 789f.events, the brand is committed to delivering a fair, responsible, and refreshing betting environment — a true breath of fresh air in the world of online entertainment.
Join today and experience the next-generation platform redefining online gaming!
32WIN is more than just an online entertainment platform — it’s the ultimate destination for those who seek challenge, excitement, and discovery.
Driven by a mission to deliver the most exceptional entertainment experiences, 32WIN continuously invests in cutting-edge technology and expands its diverse range of gaming services, ensuring every player finds something truly rewarding.
789P is one of Vietnam’s leading online betting platforms, offering a wide variety of exciting games including sports betting, live casino, and slot games.
The platform is committed to ensuring a secure and seamless betting experience by providing robust data protection and 24/7 customer support, making it a trusted destination for players across the country.
Top Reinigungsfirma in München – schnell, gründlich und preiswert
Kuwin là nền tảng cá cược trực tuyến uy tín, được cấp phép bởi chính phủ Philippines và chứng nhận bởi CEZA. Cung cấp dịch vụ đa dạng như cá cược thể thao, casino trực tuyến, và trò chơi slot, Kuwin Casino thu hút hơn 10 triệu người chơi tại Việt Nam nhờ giao diện thân thiện, dịch vụ chuyên nghiệp và nhiều ưu đãi hấp dẫn. Kuwin Direct – sự lựa chọn hàng đầu cho trải nghiệm giải trí đỉnh cao.
Helo88 là một địa chỉ cung cấp các hoạt động cá cược uy tín chất lượng đã được đông đảo thành viên tin tưởng lựa chọn. Ngoài các dịch vụ đẳng cấp nhà cái còn không ngừng cải tiến và phát triển trò chơi để mang đến nhiều sự lựa chọn cho thành viên. Nơi đây tự tự tin là nhà cái lý tưởng dành cho người chơi.
HB88 – Thế giới giải trí đỉnh cao với cá cược thể thao, casino, game bài và slot hot nhất thị trường!
Hello, I log on to your blogs regularly. Your story-telling style is witty,
keep doing what you’re doing!
Xin88 – Link Truy Cập Xin88 Chính Thức Không Chặn Mới Nhất 2025. Nạp nhanh – Rút nhanh
789WIN là nhà cái mình đang chơi hơn 3 tháng nay, thấy khá ổn. Tỷ lệ kèo cao, nhiều kèo bóng đá và casino live để lựa chọn. Giao dịch nạp rút tầm vài phút là xong, hỗ trợ cũng nhiệt tình. Anh em nào đang tìm chỗ cá cược uy tín thì thử 789WIN xem, mình thấy đáng để trải nghiệm.
789WIN – Link Truy Cập 789WINChính Thức Không Chặn Mới Nhất 2025. Nạp nhanh – Rút nhanh
HB88– Link Truy Cập HB88 Chính Thức Không Chặn Mới Nhất 2025. Nạp nhanh – Rút nhanh
32winmobi.com is the official agent of 32 Win, one of the leading online gaming platforms, offering hundreds of exciting games such as dice games (Tài Xỉu), fish shooting, slot games, and much more.
With a user-friendly interface, lightning-fast deposits and withdrawals, and 24/7 customer support, it delivers a premium gaming experience where big wins and smooth gameplay go hand in hand.
Experience top-tier entertainment – and enjoy thrilling rewards today!
HB88 – Thế giới giải trí đỉnh cao với cá cược thể thao, casino, game bài và slot hot nhất thị trường!
23WIN – Thế giới giải trí đỉnh cao với cá cược thể thao, casino, game bài và slot hot nhất thị trường!
Greetings from Idaho! I’m bored to tears at work so I decided to browse your site on my iphone
during lunch break. I love the knowledge you provide here and can’t wait to take a look when I get home.
I’m amazed at how fast your blog loaded on my cell phone ..
I’m not even using WIFI, just 3G .. Anyhow, good site!
N666 mang đến hàng loạt trò chơi trả thưởng hấp dẫn nhất năm 2025, với tỷ lệ đổi thưởng cao và giao dịch minh bạch – tạo nên uy tín vững chắc cho thương hiệu trên thị trường.
VSBET tự hào là thương hiệu giải trí online uy tín lâu đời với nền tảng công nghệ hiện đại, dịch vụ chuyên nghiệp và kho game phong phú, đáp ứng mọi nhu cầu của người chơi. Tại đây, bạn sẽ được trải nghiệm đa dạng các sản phẩm hấp dẫn như: thể thao, casino, nổ hũ, bắn cá, xổ số… cùng nhiều trò chơi đổi thưởng đỉnh cao.
Discover 23Win – a trusted online betting platform offering sports betting, live casino, slot games, and lottery.
Licensed by PAGCOR, 23Win guarantees a safe and transparent gaming environment.
Sign up today to enjoy exclusive promotions and experience world-class online entertainment at its finest!
With a user base of millions and an ever-growing community, BG678 has become a top-tier destination for online gaming in India. Its commitment to quality entertainment, fairness, and financial opportunity makes it a hub where excitement and trust go hand in hand.
66Lottery stands as a trusted destination for players seeking both entertainment and big winning opportunities.
No one wants to be stuck in a sweltering home due to a malfunctioning air conditioner.
789WIN is a trusted and legally licensed online betting platform, offering a wide range of entertainment services including sports betting, live casino, fish shooting, slot games, cockfighting, and lottery.
With its modern technology, user-friendly interface, and high-level security system, 789WIN delivers a premium, fair, and transparent betting experience.
The platform also features regularly updated promotions and 24/7 customer support, ensuring players can enjoy worry-free gaming while maximizing their chances of winning big every day.
789P is one of Vietnam’s leading and most trusted online betting platforms, offering a diverse entertainment hub with sports betting, live casino, fish shooting, jackpot slots, and many other exciting games.
Featuring a modern interface and a professional 24/7 customer support team, 789P ensures a seamless and enjoyable gaming experience for all players.
With frequently updated promotions and rewarding offers, 789P has become a top choice for seasoned bettors seeking both thrill and value.
Trên 789win, bạn có thể dễ dàng tìm thấy nhiều loại game khác nhau, từ thể thao đến casino ảo.
789WIN is a trusted and legally licensed online betting platform, offering a wide range of entertainment services including sports betting, live casino, fish shooting, slot games, cockfighting, and lottery.
With its modern technology, user-friendly interface, and high-level security system, 789WIN delivers a premium, fair, and transparent betting experience.
The platform also features regularly updated promotions and 24/7 customer support, ensuring players can enjoy worry-free gaming while maximizing their chances of winning big every day.
LINK TRUY CẬP TRANG CHỦ XIN 88 UY TÍN 2025 LÌ XÌ +88K
LINK TRUY CẬP TRANG CHỦ KUWIN tặng 188K
LINK TRUY CẬP TRANG CHỦ HB88 Bú Vội 88K + 200% Nạp Đầu
UU88 là điểm đến lý tưởng cho những ai đam mê cá cược thể thao, casino live, slot và game bắn cá đổi thưởng.
Kbet is one of Vietnam’s leading online betting platforms, well-known for offering a wide range of services including sports betting, live casino, and diverse entertainment games.
Players can wager on popular sports such as football, basketball, and tennis, while also enjoying exciting casino games like baccarat, blackjack, and a variety of card games.
In addition, Kbet features lottery games and engaging electronic entertainment options such as slot machines and fish shooting games, delivering a diverse and thrilling gaming experience for users.
LINK TRUY CẬP TRANG CHỦ SP8 Bú Nạp Đầu 188%
LINK TRUY CẬP TRANG CHỦ KUBET Bú Nạp Đầu 188%
RWIN offers a wide range of online casino games, designed to suit players of all levels. With hundreds of diverse game options, the platform not only delivers endless entertainment but also provides attractive rewards and exclusive promotions tailored for its members.
U888 is a leading online betting platform in Vietnam, well-known for its high-quality casino halls and thousands of rewarding games.
New players who register an account will instantly receive a ₫88,000 bonus, along with the opportunity to claim many other valuable promotional rewards.
RR88 is one of Asia’s most trusted online betting platforms, fully licensed by the Isle of Man and the UK Gambling Commission.
Featuring a diverse game library including casino, sports betting, fish shooting, slot games, and lottery, RR88 stands out with GEOTRUST-certified security, a user-friendly interface, and 24/7 customer support.
🎁 Register now to claim bonuses of up to ₫888,000 and enjoy a safe, transparent, and premium betting experience.
Banca30 operates under a legal license and strictly complies with the standards of the Philippine Amusement and Gaming Corporation (PAGCOR) — one of Asia’s most reputable authorities in the online entertainment industry. This ensures that all activities are conducted in a transparent, fair, and secure manner for players.
With PAGCOR’s supervision, Banca30 is committed to providing an international-standard online gaming environment, offering absolute data security and a diverse range of products, allowing players to enjoy and engage with confidence over the long term.
J88 is one of the most reputable online betting brands in Vietnam, legally licensed by the Government of Costa Rica.
With a diverse and constantly updated game library, J88 is committed to delivering a premium entertainment experience that meets the needs of every betting enthusiast.
MM88 is one of Asia’s leading online betting platforms, delivering a fair and transparent entertainment experience with a vast game library that includes sports betting, live casino, cockfighting, lottery, fish shooting, and slot games.
Launched in 2006 and operated by Loom Club LTD in the Philippines, MM88 is fully licensed by PAGCOR, the Isle of Man, and MGA, earning the trust of over 10 million members worldwide.
With modern technology, a user-friendly interface, and valuable promotions, MM88 has become the go-to destination for Vietnamese players seeking both excitement and security.
This article provides a detailed look at MM88, including its history, legal background, advantages, products, promotions, participation guide, FAQs, and expert tips to maximize your winnings in 2025.
Discover 23Win – a trusted online betting platform offering sports betting, live casino, slot games, and lottery.
Licensed by PAGCOR, 23Win ensures a safe, secure, and transparent gaming environment for all players.
🎯 Sign up today to claim exclusive promotions and experience world-class online entertainment at its finest!
Link đăng nhập – đăng ký HB88 chuẩn nhất 2025 [ Không bị chặn ] — Tặng lì xì 88k
Excellent breakdown of the topic.
32Win is a leading and trusted online betting platform, offering a wide variety of services including sports betting, live casino, slot games, and lottery.
Licensed by PAGCOR, 32Win ensures a safe, transparent, and secure gaming environment for every player.
🎯 Join today to enjoy exclusive promotions and experience world-class online entertainment like never before!
32Win is a trusted online entertainment website, specializing in sports betting, live casino, and a variety of reward-based games.
With its user-friendly interface and a diverse game selection, 32Win delivers an engaging and enjoyable gaming experience for all players.
The platform also places strong emphasis on security and customer support, complemented by exclusive promotions and professional service, ensuring a safe and rewarding environment for every user.
32Win is a trusted online entertainment website, specializing in sports betting, live casino, and a variety of reward-based games.
With its user-friendly interface and a diverse game selection, 32Win delivers an engaging and enjoyable gaming experience for all players.
The platform also places strong emphasis on security and customer support, complemented by exclusive promotions and professional service, ensuring a safe and rewarding environment for every user.
Nohu90 is a trusted online entertainment platform, specializing in sports betting, live casino, and a variety of reward-based games.
With its user-friendly interface and a wide selection of games, Nohu90 offers players an engaging and enjoyable gaming experience.
The platform also prioritizes security and customer support, complemented by exclusive promotions and professional service, ensuring a safe, reliable, and rewarding environment for every user.
The choice of whether to use WITH-SLOTS versus WITH-ACCESSORS is the same as the choice between SLOT-VALUE and an accessor function: low-level code that provides the basic functionality of a class may use SLOT-VALUE or WITH-SLOTS to directly manipulate slots in ways not supported by accessor functions or to explicitly avoid the effects of auxiliary methods that may have been defined on the accessor functions. SLOT-VALUE takes an object and the name of a slot as arguments and returns the value of the named slot in the given object. But if you don’t supply a :customer-name argument, the customer-name slot will be unbound, and an attempt to read it before you set it will signal an error. Nginx has a concept of request processing time – time elapsed since the first bytes were read from the client. You can also use initforms that generate a different value each time they’re evaluated–the initform is evaluated anew for each object. For now, however, you’re ready to take a break from all this theory of object orientation and turn to the rather different topic of how to make good use of Common Lisp’s powerful, but sometimes cryptic, FORMAT function. In Chapter 23 you’ll see an example of how to define a method on PRINT-OBJECT to make objects of a certain class be printed in a more informative form.
🎰 Slot Games at RR88
RR88 offers a wide variety of exciting slot titles such as Mega Jackpot, Star Spins, and Lucky Wheels, featuring high payout rates and random jackpot features that keep every spin thrilling.
🃏 Live Casino
Enjoy real-time gaming with tables for Baccarat, Dragon Tiger, Sic Bo, and Poker, all streamed directly from international studios, ensuring a realistic and professional casino experience.
⚽ Sports Betting
With over 1,000 daily matches, RR88 covers a broad range of sports including football, basketball, and eSports, giving players diverse betting options every day.
Nhà Cái Uy Tín is a trusted platform that aggregates, reviews, and introduces reputable online betting sites in both Vietnam and Asia.
With the principles of objectivity, transparency, and timely updates, the website helps players easily access accurate information about bookmakers, betting odds, promotions, and the latest login links.
Whether you are a beginner exploring online betting or an experienced player looking to compare and choose, nhacaiuytin.net.ph is the ideal resource to guide your decisions.
keonhacai.now is a leading website specializing in providing up-to-date football betting odds and bookmaker lines, serving the information needs of passionate sports fans.
Born from a love of sports, keonhacai.now delivers detailed match schedules, results, standings, and the latest sports news. With a team of experienced experts, the platform also offers accurate match previews and betting insights.
At keonhacai.now, you’ll find all the popular betting markets such as Asian Handicap, European Odds, and more — helping you make smarter decisions while following your favorite matches.
OK9 được biết đến như một trong những nhà cái cá cược trực tuyến uy tín tại Việt Nam, nơi hội tụ đầy đủ các sản phẩm giải trí hiện đại: cá cược thể thao, casino online, bắn cá, nổ hũ, đá gà, lô đề. Người chơi có thể dễ dàng đăng ký tài khoản OK9, trải nghiệm giao diện thân thiện trên cả web và app mobile, cùng hệ thống tỷ lệ kèo châu Á, kèo châu Âu chuẩn xác. Bên cạnh đó, OK9 còn nổi bật với khuyến mãi hấp dẫn, nạp rút siêu tốc và dịch vụ chăm sóc khách hàng 24/7, đảm bảo mang đến trải nghiệm an toàn – minh bạch cho mọi bet thủ.
U888 là nhà cái cá cược trực tuyến hàng đầu tại Việt Nam, nổi bật với nổ hũ đổi thưởng tỷ lệ cao, cùng hệ sinh thái game đa dạng: cá cược thể thao, casino live, bắn cá, đá gà, xổ số, và eSports. Với giấy phép quốc tế, U888 đảm bảo an toàn, minh bạch và dịch vụ khách hàng chuẩn 5 sao.
Link đăng nhập – dăng ký nhà cái HB88 uy tín mới nhất hiện tại !
Mình chơi ở HB88 lâu rồi, thấy tỷ lệ kèo minh bạch, nhiều trò chơi đa dạng và thanh toán an toàn, đáng để tin tưởng.
siteniz çok güzel devasa bilgilendirme var aradığım herşey burada mevcut çok teşekkür ederim
Fly88 – Vương Quốc Hoàng Kim, Thắng Lớn Như Vua, Ưu Đãi Hàng Ngày!
Fly88 – Vận May Bất Tận, Cá Cược Siêu Tốc, Thưởng Đăng Ký!
OK9 – Sân Chơi Hoàn Hảo, Chiến Thắng Kép, Thưởng Hấp Dẫn!
OK9 mang đến ứng dụng tiện lợi trên cả Android và iOS, cho phép bạn đặt cược linh hoạt mọi lúc, mọi nơi. Giao diện thân thiện, được tối ưu hóa với hiệu suất mượt mà, đảm bảo trải nghiệm cá cược đỉnh cao.
OK9 Cung cấp đa dạng các hình thức cá cược từ thể thao, casino trực tuyến, đá gà, nổ hũ, xổ số, eSports, live casino…
OK9 – Hỗ trợ 24/7 qua nhiều kênh: live chat, email, điện thoại, Telegram, mạng xã hội, hotline… với đội ngũ nhân viên dày dặn
Nhà cái uy tín OK9 có giấy phép từ các tổ chức quản lý cá cược quốc tế như: PAGCOR (Philippines), Curacao, MGA (Malta Gaming Authority), Isle of Man, v.v.
Fly88 cung cấp cho người chơi một môi trường cá cược an toàn, tiện lợi, có thể tham gia từ bất kỳ đâu chỉ cần có kết nối internet.
Fly88 – điểm đến đỉnh cao cho những tín đồ cá cược, mang đến hàng loạt sảnh cược phong phú, công nghệ hiện đại hàng đầu và dịch vụ hỗ trợ chu đáo
OK9 – thiên đường cá cược dành cho anh em đam mê, hội tụ vô vàn sảnh cược đa dạng, công nghệ tối tân và dịch vụ hỗ trợ tận tình, luôn sẵn sàng nâng tầm trải nghiệm của bạn!
Incredible! This blog looks exactly like my old one!
It’s on a completely different topic but it has pretty much the same layout and design. Great choice of colors!
Hello, I want to subscribe for this blog to get most up-to-date updates, therefore where can i do it please assist.
Thanks very nice blog!
OK9.COM là nền tảng cá cược sở hữu công nghệ tiên tiến, bảo mật 256-bit, và tốc độ truy cập cực nhanh kể cả khi mạng yếu. Tại đây, người chơi có thể đặt cược mọi lúc, không cần lo chuyện chặn IP hay giới hạn địa lý.
OK9 – Vận May Bất Tận, Cá Cược Siêu Tốc, Thưởng Đăng Ký Khủng!
Hi there mates, pleasant article and good arguments commented at this place, I am really enjoying by
these.
OK9 – Cổng Game CASINO 5 Sao Quốc Tế 2025
Nice response in return of this question with genuine
arguments and describing the whole thing regarding that.
Khám Phá Nhà Cái Hàng Đầu – Trải Nghiệm Cá Cược Đỉnh Cao!
NEW88 is the leading reputable online betting platform in the Vietnamese market. It offers a wide range of rewarding games, including sports betting, slots, fish shooting, and lottery.
The reputable betting house NEW88 has proven its dominance, emerging as one of the premier and most dependable entertainment destinations in Vietnam today.
NEW88, the esteemed bookmaker, has solidified its stature as one of Vietnam’s most trustworthy entertainment hubs in the current landscape.
Milanobet’in güncel giriş adresini sitemizde bulabilirsiniz. Siz de kaliteli bahis heyecanı yaşamak istiyorsanı hemen Milanobet’e üye olun!
With unwavering credibility, MB66 has cemented its place among Vietnam’s top reliable entertainment platforms, captivating players nationwide right now.
MB66 Thailand offers a promotion of 88 baht for first-time registered customers.
MB66 Thailand warmly welcomes new customers with an exclusive 88 baht bonus upon their first registration, unlocking a thrilling start to their gaming journey.
Tarabet hakkında merak ettiğiniz tüm konular bizim sitemizde!
MB66 Thailand welcomes first-time players with a free 88 baht bonus – start winning today!
FLY88 – nhà cái cá cược online mới hoạt động hợp pháp tại Việt Nam, mang đến kho trò chơi hấp dẫn cùng nhiều khuyến mãi siêu hời.
вулкан казино
казино вулкан
вулкан рояль
vulcan casino
вулкан рояль кз
I don’t even know how I ended up here, but I
thought this post was great. I don’t know who you are but definitely you’re going to
a famous blogger if you are not already 😉 Cheers!
Wow, fantastic blog layout! How long have you been blogging for?
you make blogging look easy. The overall look of your site is
wonderful, let alone the content!
**mind vault**
Mind Vault is a premium cognitive support formula created for adults 45+. It’s thoughtfully designed to help maintain clear thinking
**mindvault**
Mind Vault is a premium cognitive support formula created for adults 45+. It’s thoughtfully designed to help maintain clear thinking
Lương Sơn TV stream nhanh, không bị văng ra dù xem hơn 90 phút, giao diện web dễ chọn giải đấu, có lịch rõ ràng — fan Premier League như mình cực kỳ thích.
Bahis sitelerinde sunulan bonuslar genellikle belli şartlar altında verilir. Örneğin, hoş geldin bonusları genellikle ilk üyelik işlemi sonrasında verilir ve belli bir yatırım şartını içerebilir. Kayıp bonusları ise belirli bir miktarın üzerinde kayıp yaşandığında verilir ve genellikle belli bir yatırım şartını gerektirmez.
Mình xem bóng đá trên LuongSonTV suốt mấy tháng nay, phải nói tốc độ load cực nhanh, gần như không bị giật dù xem trên điện thoại hay laptop. Hình ảnh rõ, âm thanh ổn, đặc biệt là không có quảng cáo pop-up nên cảm giác rất thoải mái. Nền tảng này xứng đáng nằm top trong các trang xem bóng đá online hiện nay.
Trước giờ mình thử qua nhiều trang xem bóng đá, nhưng Luongsontv là nơi mình gắn bó lâu nhất. Link ổn định, BLV vui tính mà vẫn có chuyên môn, lịch thi đấu và highlight cập nhật nhanh. Quan trọng là web hoạt động uy tín, không chèn quảng cáo khó chịu. Rất đáng tin để xem mỗi cuối tuần.
Milanobet, lisanslı bir bahis sitesi olarak kullanıcılarına güvenilir bir oyun ortamı sunmaktadır. Lisanslı olması, siteye üye olan kullanıcıların kişisel ve finansal bilgilerinin güvende olduğunu göstermektedir. Ayrıca, lisanslı bir site olarak Milanobet, kullanıcıların adil bir oyun deneyimi yaşamasını da sağlamaktadır.
บทความนี้ให้ข้อมูลมีประโยชน์มากครับ ถ้าใครกำลังมองหาบริการจัดดอกไม้งานศพ ผมแนะนำลองดูร้านที่มีผลงานจริงและรีวิวดี ๆ ครับ
Write more, thats all I have to say. Literally, it seems as
though you relied on the video to make your point. You definitely know what youre talking about, why throw away your intelligence
on just posting videos to your blog when you could
be giving us something enlightening to read?
Excellent way of describing, and nice piece of writing to take
information on the topic of my presentation subject, which i am going to deliver in school.
Lương Sơn TV có giao diện dễ dùng, tìm trận đấu nhanh trong vài giây. Phù hợp với người lớn tuổi cũng dễ thao tác.
Thanks a lot! A lot of info.
You reported this terrifically.
Milanobet ile sen de kazan!
Mình thích nhất là BLV trên Lương Sơn TV, vừa có chuyên môn, vừa nói vui, nghe cực dễ chịu mà vẫn hiểu trận
Hello! Quick question that’s totally off
topic. Do you know how to make your site mobile friendly?
My web site looks weird when viewing from my iphone4. I’m trying to
find a theme or plugin that might be able to correct this problem.
If you have any recommendations, please share. Thanks!
I blog frequently and I truly appreciate your information. Your article
has really peaked my interest. I will book mark your blog and
keep checking for new details about once per week.
I subscribed to your RSS feed as well.
Heya i am for the first time here. I found this board and I find It truly useful & it helped
me out a lot. I hope to give something back and aid others like you aided me.
Điểm mình thích nhất ở luongsontv là xem truc tiep bong da trên điện thoại rất mượt, không có quảng cáo che kín màn hình như một số trang làm rất phiền. Ngồi đâu cũng xem được, chỉ cần bật là có trận. Dân xem bóng di động nên thử.
Have you ever thought about publishing an ebook or guest authoring on other blogs?
I have a blog based on the same subjects you discuss and would really like to have you share some stories/information. I know my readers would value your
work. If you’re even remotely interested, feel free to send me an e-mail.
My coder is trying to persuade me to move to .net from PHP.
I have always disliked the idea because of the costs.
But he’s tryiong none the less. I’ve been using Movable-type on a variety of websites for about a year and am concerned about
switching to another platform. I have heard fantastic
things about blogengine.net. Is there a way I can transfer all my wordpress
posts into it? Any help would be really appreciated!
Does your site have a contact page? I’m having problems locating it but, I’d like to shoot you an email.
I’ve got some recommendations for your blog you might be interested in hearing.
Either way, great site and I look forward to seeing
it develop over time.
It’s great that you are getting thoughts from this piece of writing as well as
from our discussion made at this time.
Поездка — это не просто вариант переместиться, а предсказуемое сопровождение в пути для тех, кто ценит своё спокойствие.
**Фиксированная и выгодная стоимость трансфера — никаких сюрпризов!** Вы переводите ровно ту стоимость, которая была указана при резервировании — без непредвиденных расходов.
Компания работает круглосуточно, обеспечивая мгновенный прибытие. непредвиденные обстоятельства — больше не ваша забота.
Вы можете наблюдать локацию машины в живом режиме, заранее узнавать профиль курьера и бронировать оптимальный класс машины — от бюджетного до премиума.
Бронируйте заранее — и вы минимизируете напряжения. Это идеально подходит для путешествий в хаб, на конференции, к друзьям или просто для комфортного передвижения.
Профессионализм, открытость и внимание к деталям — вот что делает ваш маршрут по-настоящему выгодным.
I will immediately grasp your rss as I can not in finding your e-mail subscription link or newsletter service.
Do you have any? Kindly permit me recognize so that I may just subscribe.
Thanks.
Сервис обслуживает 24/7, гарантируя быстрый отклик. Вам не нужно нервничать о непредвиденных обстоятельствах — курьер учтёт все обстоятельства маршрута.
Вы можете отслеживать местоположение средства передвижения в онлайн, заранее изучить информацию водителя и назначить оптимальный уровень транспорта — от бюджетного до премиума.
Резервируйте заблаговременно — и вы избежите ожидания. Это наилучшим образом подходит для рейсов в вокзал, на мероприятия, к друзьям или просто для лёгкого перемещения.
Безопасность, честность и индивидуальный подход — вот что делает ваш маршрут по-настоящему выгодным.
Great blog! Is your theme custom made or did you download it from somewhere?
A theme like yours with a few simple adjustements would really make my blog shine.
Please let me know where you got your theme. Thanks
I love reading this article so beautiful!!great job!
Hurrah! After all I got a website from where I know how to in fact
take helpful facts concerning my study and knowledge.
I was curious if you ever considered changing the layout of your website?
Its very well written; I love what youve got to
say. But maybe you could a little more in the way of content so people
could connect with it better. Youve got an awful lot of text for only having one or 2 images.
Maybe you could space it out better?
Heya are using WordPress for your site platform? I’m new to the blog world
but I’m trying to get started and create my own. Do you require any html coding knowledge to make your own blog?
Any help would be greatly appreciated!
My brother recommended I might like this website. He was entirely right.
This post truly made my day. You can not imagine simply how
much time I had spent for this info! Thanks!
Good day! I know this is kinda off topic but I’d figured I’d ask.
Would you be interested in exchanging links or maybe guest writing a blog article or vice-versa?
My blog discusses a lot of the same subjects as yours
and I believe we could greatly benefit from each other.
If you might be interested feel free to shoot me an email.
I look forward to hearing from you! Wonderful blog by the way!
Vegabet ile tüm maçlar her an yanınızda.
After exploring a few of the blog articles on your site, I honestly appreciate your technique of blogging.
I saved it to my bookmark site list and will be checking back
soon. Please check out my website as well and
let me know how you feel.
This is a really good tip especially to those new to the blogosphere.
Simple but very precise information… Many thanks for sharing this one.
A must read post!
Pretty nice post. I simply stumbled upon your blog and wanted to mention that I’ve truly loved browsing your weblog posts.
After all I will be subscribing to your feed and I am hoping
you write again soon!
Currently it sounds like BlogEngine is the preferred blogging platform available
right now. (from what I’ve read) Is that what you’re using on your blog?
Hi to every one, the contents present at this site are truly amazing for
people experience, well, keep up the nice work fellows.
Hi there, i read your blog occasionally and i own a similar one
and i was just wondering if you get a lot of spam comments?
If so how do you reduce it, any plugin or anything you can suggest?
I get so much lately it’s driving me insane so any assistance
is very much appreciated.
Thanks for sharing your info. I truly appreciate your efforts and I will be waiting
for your further post thank you once again.
Oh my goodness! Awesome article dude! Thank you, However I am experiencing issues with your RSS.
I don’t understand why I can’t join it. Is there anyone
else having similar RSS issues? Anyone that knows
the solution will you kindly respond? Thanks!!
Hi there! I know this is somewhat off-topic however I needed to ask.
Does managing a well-established blog such as yours take a lot of work?
I’m completely new to running a blog however I do write in my diary daily.
I’d like to start a blog so I will be able to share my experience
and feelings online. Please let me know if you have any kind of recommendations or tips for brand new aspiring bloggers.
Appreciate it!
Awesome! Its truly amazing paragraph, I have got much clear idea on the topic of from
this post.
Attractive part of content. I simply stumbled upon your web site and in accession capital to assert that I get
in fact enjoyed account your blog posts. Anyway I’ll be subscribing on your augment or even I
achievement you get entry to persistently rapidly.
Wow, amazing blog layout! How long have you been blogging for?
you made blogging look easy. The overall look of your site is excellent, as well as the
content!
Hi there, just became alert to your blog through Google, and found
that it’s truly informative. I’m gonna watch out for brussels.
I will be grateful if you continue this in future.
Numerous people will be benefited from your
writing. Cheers!
Saved as a favorite, I love your web site!
I think the admin of this webb page is actually worfking hard for
hiss website, as here every information is quality based
information.
Thanks for sharing your thoughts. I really appreciate your efforts and I am waiting for
your further post thank you once again.
Have you ever thought about writing an e-book or guest authoring on other websites?
I have a blog based upon on the same subjects you discuss and would love to have you
share some stories/information. I know my readers would value
your work. If you are even remotely interested, feel free to shoot me an e-mail.
Hi, this weekend is pleasant in favor of me, as this point iin time i
am reading this impressie informative article here at myy house.
What’s up to every one, the contents present
at this site are in fact remarkable for people knowledge,
well, keep up the nice work fellows.
It’s an remarkable article designed for all the web viewers; they will take advantage from it I am sure.
I was suggested this website through my cousin. I’m no longer positive whether or not this publish is
written by him as no one else understand such certain approximately my trouble.
You’re incredible! Thanks!
My brother recommended I may like this blog.
He was once entirely right. This publish actually made
my day. You cann’t believe just how a lot time I had spent
for this information! Thanks!
Keep this going please, great job!
What’s up colleagues, how is all, and what you wish for to say on the topic of
this piece of writing, in my view its actually awesome in favor of me.
We are a group of volunteers and opening a new scheme in our community.
Your website provided us with valuable information to work on. You’ve done
a formidable job and our whole community will be grateful
to you.
I can’t wait for your next post.
Köszönöm hogy időt szántál ennek megírására.
I think this is one of the most vital info for me. And i am glad reading
your article. But should remark on some general things,
The web site style is wonderful, the articles is really excellent : D.
Good job, cheers
Great article, totally what I was looking for.
Hi! I know this is kinda off topic but I was wondering if
you knew where I could find a captcha plugin for my comment form?
I’m using the same blog platform as yours and I’m having difficulty
finding one? Thanks a lot!
Greetings from Los angeles! I’m bored to death at work so I decided to check out your site
on my iphone during lunch break. I really like the info you
provide here and can’t wait to take a look when I get home.
I’m shocked at how fast your blog loaded on my mobile ..
I’m not even using WIFI, just 3G .. Anyhow, wonderful site!
Hi, Neat post. There’s a problem along with your website in internet explorer, would test this?
IE nonetheless is the market leader and a good portion of other folks will
omit your great writing because of this problem.
I’m now not sure where you’re getting your information,
but great topic. I must spend a while studying
much more or working out more. Thank you for wonderful info I
was looking for this info for my mission.
I don’t even know how I ended up here, but I thought this post was good.
I do not know who you are but definitely you’re going
to a famous blogger if you aren’t already ;
) Cheers!
What’s up, I read your blog on a regular basis. Your humoristic style is
witty, keep up the good work!
I just couldn’t depart your website before suggesting that I actually
loved the usual info an individual provide for your guests?
Is going to be back incessantly in order to check up on new posts
I’ve been exploring for a little bit for any high quality
articles or blog posts in this kind of house
. Exploring in Yahoo I finally stumbled upon this
site. Reading this information So i am glad to express that I have an incredibly good uncanny feeling I came upon just
what I needed. I such a lot no doubt will make sure to do not fail to remember this website and
give it a glance on a continuing basis.
Wow, incredible blog format! How lengthy have you been running
a blog for? you made blogging glance easy. The total look of your website is excellent,
let alone the content!
Luar biasa artikelnya! Inflasi yang stabil sangat membantu menjaga konsumsi rumah tangga.
Jarang ada artikel yang mengulas ini secara netral dan lengkap.
Jangan lupakan juga bursa judi bola terlengkap yang makin ramai
di tengah stabilitas ekonomi.
Artikel ini bisa jadi referensi bagus, termasuk untuk pelaku
situs judi bola terlengkap dan terpercaya.
Thanks sudah berbagi artikel berkualitas seperti ini!
I’d like to thank you for the efforts you’ve put in penning this site.
I’m hoping to check out the same high-grade content by you in the
future as well. In fact, your creative writing abilities has inspired
me to get my own site now 😉
Very energetic post, I enjoyed that a lot. Will there be
a part 2?
Hi there would you mind sharing which blog platform you’re working with?
I’m planning to start my own blog in the near future but I’m having a hard
time making a decision between BlogEngine/Wordpress/B2evolution and
Drupal. The reason I ask is because your layout seems different then most blogs and I’m looking for something
completely unique. P.S My apologies for getting off-topic but I had to ask!
Nice post. I was checking continuously this
weblog and I am inspired! Very useful information specially the final section 🙂 I take
care of such info much. I was looking for this particular information for
a long time. Thank you and best of luck.
Pretty! This has been a really wonderful post. Thank you for providing this information.
I really like it when people come together and share thoughts.
Great site, continue the good work!
naturally like your web-site but you have to test the
spelling on several of your posts. Many of them are
rife with spelling problems and I find it very troublesome to tell the reality on the other hand I will certainly come back again.
저희 인천출장마사지는 고객님이 가장 편안함을 느끼는 곳으로 직접 찾아가, 불필요한 이동 없이 오롯이 휴식에만 집중할 수 있도록 도와드립니다. 자택, 숙소, 오피스텔 인천출장마사지 등
Компания функционирует 24/7, гарантируя быстрый отклик. Вам не нужно беспокоиться о пробках — специалист адаптируется к все нюансы перемещения.
Вы можете контролировать положение транспорта в непосредственно, заранее узнать характеристики шофёра и подобрать соответствующий категорию машины — от бюджетного до люкса.
Заказывайте вовремя — и вы избежите стресса. Это безупречно подходит для путешествий в хаб, на деловые встречи, к партнёрам или просто для расслабленного перемещения.
Безопасность, честность и учёт пожеланий — вот что делает ваш трансфер по-настоящему важным.
The samples made it click.
Thanks for sharing the info, keep up the good work going…. I really enjoyed exploring your site. good resource…
I found your this post while searching for some related information on blog search…Its a good post..keep posting and update the information.
(10 euros gratis apuestas|10 mejores casas de apuestas|10 trucos para ganar apuestas|15 euros gratis marca apuestas|1×2 apuestas|1×2 apuestas deportivas|1×2
apuestas que significa|1×2 en apuestas|1×2 en apuestas que
significa|1×2 que significa en apuestas|5 euros gratis apuestas|9 apuestas que siempre ganaras|a
partir de cuanto se declara apuestas|actividades de
juegos de azar y apuestas|ad apuestas deportivas|aleksandre topuria ufc apuestas|algoritmo para ganar apuestas deportivas|america
apuestas|análisis nba apuestas|aplicacion android apuestas deportivas|aplicacion apuestas deportivas|aplicacion apuestas deportivas android|aplicación de apuestas online|aplicacion para hacer apuestas|aplicacion para hacer apuestas de
futbol|aplicación para hacer apuestas de fútbol|aplicaciones apuestas deportivas
android|aplicaciones apuestas deportivas gratis|aplicaciones de apuestas android|aplicaciones de
apuestas de fútbol|aplicaciones de apuestas deportivas|aplicaciones de apuestas deportivas peru|aplicaciones de apuestas deportivas perú|aplicaciones de apuestas en colombia|aplicaciones de apuestas gratis|aplicaciones de apuestas online|aplicaciones de apuestas
seguras|aplicaciones de apuestas sin dinero|aplicaciones
para hacer apuestas|apostar seguro apuestas deportivas|app android apuestas deportivas|app apuestas|app apuestas android|app apuestas de
futbol|app apuestas deportivas|app apuestas deportivas android|app apuestas deportivas argentina|app apuestas deportivas colombia|app apuestas deportivas ecuador|app apuestas deportivas españa|app apuestas deportivas gratis|app
apuestas entre amigos|app apuestas futbol|app apuestas gratis|app apuestas sin dinero|app casa
de apuestas|app casas de apuestas|app control apuestas|app de apuestas|app de apuestas android|app de apuestas casino|app de apuestas
colombia|app de apuestas con bono de bienvenida|app de apuestas de futbol|app de apuestas deportivas|app de apuestas deportivas android|app de apuestas deportivas argentina|app de apuestas deportivas colombia|app de apuestas
deportivas en españa|app de apuestas deportivas peru|app de apuestas deportivas
perú|app de apuestas deportivas sin dinero|app
de apuestas ecuador|app de apuestas en colombia|app de apuestas en españa|app de apuestas en venezuela|app de apuestas futbol|app de apuestas gratis|app de apuestas online|app
de apuestas para android|app de apuestas para ganar dinero|app de apuestas peru|app de
apuestas reales|app de casas de apuestas|app marca apuestas android|app
moviles de apuestas|app para apuestas|app para apuestas de
futbol|app para apuestas deportivas|app para apuestas deportivas en español|app para ganar apuestas deportivas|app para hacer apuestas|app
para hacer apuestas deportivas|app para hacer apuestas entre amigos|app para llevar control
de apuestas|app pronosticos apuestas deportivas|app versus apuestas|apps apuestas mundial|apps de apuestas|apps
de apuestas con bono de bienvenida|apps de apuestas
de futbol|apps de apuestas deportivas peru|apps de
apuestas mexico|apps para apuestas|aprender a hacer apuestas deportivas|aprender hacer apuestas deportivas|apuesta del dia apuestas deportivas|apuestas 10
euros gratis|apuestas 100 seguras|apuestas 1×2|apuestas 1X2|apuestas 2 division|apuestas
3 division|apuestas a caballos|apuestas a carreras de caballos|apuestas a colombia|apuestas a corners|apuestas a ganar|apuestas a jugadores nba|apuestas a la baja|apuestas a la nfl|apuestas al barcelona|apuestas al dia|apuestas
al empate|apuestas al mundial|apuestas al tenis wta|apuestas alaves barcelona|apuestas alcaraz hoy|apuestas alemania españa|apuestas alonso campeon del mundo|apuestas altas y bajas|apuestas altas y bajas nfl|apuestas ambos equipos
marcan|apuestas america|apuestas android|apuestas anillo nba|apuestas antes del mundial|apuestas anticipadas|apuestas anticipadas
nba|apuestas apps|apuestas arabia argentina|apuestas
argentina|apuestas argentina campeon del mundo|apuestas argentina canada|apuestas argentina colombia|apuestas argentina croacia|apuestas argentina españa|apuestas argentina francia|apuestas argentina francia cuanto paga|apuestas
argentina francia mundial|apuestas argentina gana el mundial|apuestas argentina gana mundial|apuestas argentina
holanda|apuestas argentina mexico|apuestas argentina méxico|apuestas argentina mundial|apuestas argentina online|apuestas argentina
paises bajos|apuestas argentina polonia|apuestas argentina uruguay|apuestas argentina vs australia|apuestas argentina vs colombia|apuestas argentina vs francia|apuestas argentina vs peru|apuestas argentinas|apuestas arsenal real
madrid|apuestas ascenso a primera division|apuestas ascenso
a segunda|apuestas asiaticas|apuestas asiatico|apuestas athletic|apuestas athletic atletico|apuestas
athletic barça|apuestas athletic barcelona|apuestas athletic
betis|apuestas athletic manchester|apuestas athletic manchester united|apuestas athletic
osasuna|apuestas athletic real|apuestas athletic real madrid|apuestas athletic real sociedad|apuestas athletic real sociedad final|apuestas athletic roma|apuestas athletic sevilla|apuestas athletic
valencia|apuestas atletico|apuestas atletico barcelona|apuestas atletico
barsa|apuestas atletico campeon champions|apuestas atletico campeon de liga|apuestas atlético copenhague|apuestas atletico de madrid|apuestas atlético de madrid|apuestas atletico de madrid barcelona|apuestas atletico de
madrid gana la liga|apuestas atletico de madrid real madrid|apuestas atlético de madrid real madrid|apuestas atletico de madrid vs barcelona|apuestas atletico madrid|apuestas atletico madrid real madrid|apuestas atletico madrid
vs barcelona|apuestas atletico real madrid|apuestas atletico real madrid champions|apuestas
atletismo|apuestas bajas|apuestas baloncesto|apuestas baloncesto acb|apuestas baloncesto handicap|apuestas baloncesto
hoy|apuestas baloncesto juegos olimpicos|apuestas baloncesto nba|apuestas baloncesto pronostico|apuestas
baloncesto pronósticos|apuestas baloncesto prorroga|apuestas barca|apuestas barca athletic|apuestas barca atletico|apuestas barca bayern|apuestas barca bayern munich|apuestas barca girona|apuestas barca hoy|apuestas
barça hoy|apuestas barca inter|apuestas barca juventus|apuestas barca madrid|apuestas barça madrid|apuestas barca real madrid|apuestas barca vs juve|apuestas
barca vs madrid|apuestas barca vs psg|apuestas barcelona|apuestas barcelona alaves|apuestas barcelona athletic|apuestas barcelona atletico|apuestas
barcelona atletico de madrid|apuestas barcelona
atlético de madrid|apuestas barcelona atletico madrid|apuestas barcelona bayern|apuestas barcelona betis|apuestas barcelona campeon de liga|apuestas
barcelona celta|apuestas barcelona espanyol|apuestas barcelona gana
la champions|apuestas barcelona girona|apuestas barcelona granada|apuestas barcelona hoy|apuestas barcelona inter|apuestas barcelona madrid|apuestas
barcelona osasuna|apuestas barcelona psg|apuestas barcelona real madrid|apuestas
barcelona real sociedad|apuestas barcelona sevilla|apuestas barcelona valencia|apuestas barcelona villarreal|apuestas
barcelona vs atletico madrid|apuestas barcelona vs madrid|apuestas barcelona vs real madrid|apuestas barsa madrid|apuestas basket hoy|apuestas bayern barcelona|apuestas bayern vs barcelona|apuestas beisbol|apuestas béisbol|apuestas beisbol mlb|apuestas beisbol pronosticos|apuestas beisbol venezolano|apuestas betis|apuestas betis – chelsea|apuestas betis barcelona|apuestas betis chelsea|apuestas betis fiorentina|apuestas
betis girona|apuestas betis madrid|apuestas betis mallorca|apuestas
betis real madrid|apuestas betis real sociedad|apuestas betis sevilla|apuestas betis valencia|apuestas betis valladolid|apuestas betis
vs valencia|apuestas betplay hoy colombia|apuestas betsson peru|apuestas bienvenida|apuestas billar online|apuestas bolivia vs colombia|apuestas bono|apuestas bono bienvenida|apuestas
bono de bienvenida|apuestas bono de bienvenida sin deposito|apuestas bono gratis|apuestas bono sin deposito|apuestas
bonos sin deposito|apuestas borussia real madrid|apuestas boxeo|apuestas boxeo de campeonato|apuestas
boxeo españa|apuestas boxeo español|apuestas boxeo femenino olimpiadas|apuestas
boxeo hoy|apuestas boxeo online|apuestas brasil colombia|apuestas brasil
peru|apuestas brasil uruguay|apuestas brasil vs colombia|apuestas brasil vs peru|apuestas caballos|apuestas caballos colocado|apuestas
caballos españa|apuestas caballos hipodromo|apuestas caballos hoy|apuestas caballos madrid|apuestas caballos online|apuestas caballos sanlucar de barrameda|apuestas caballos zarzuela|apuestas calculador|apuestas campeon|apuestas campeon champions|apuestas campeón champions|apuestas campeon champions 2025|apuestas campeon champions league|apuestas campeon conference league|apuestas
campeon copa america|apuestas campeon copa del rey|apuestas campeon de champions|apuestas campeon de la champions|apuestas campeon de liga|apuestas campeon del mundo|apuestas campeon eurocopa|apuestas campeón eurocopa|apuestas campeon europa league|apuestas campeon f1|apuestas campeon f1 2025|apuestas campeon formula 1|apuestas campeon libertadores|apuestas campeon liga|apuestas campeon liga bbva|apuestas campeon liga española|apuestas campeon liga santander|apuestas campeon motogp 2025|apuestas campeon mundial|apuestas campeón mundial|apuestas campeon mundial baloncesto|apuestas campeon nba|apuestas campeón nba|apuestas campeon premier|apuestas
campeon premier league|apuestas campeon roland garros|apuestas campeonato f1|apuestas campeonatos
de futbol|apuestas carrera de caballos|apuestas carrera de caballos hoy|apuestas carrera de caballos
nocturnas|apuestas carrera de galgos fin de semana|apuestas carrera de galgos hoy|apuestas carrera
de galgos nocturnas|apuestas carreras caballos|apuestas
carreras caballos sanlucar|apuestas carreras de caballos|apuestas carreras de caballos en directo|apuestas carreras de caballos en vivo|apuestas carreras de caballos españa|apuestas carreras de caballos hoy|apuestas carreras de
caballos nacionales|apuestas carreras de caballos nocturnas|apuestas carreras de caballos
online|apuestas carreras de caballos sanlucar|apuestas carreras de caballos sanlúcar|apuestas carreras de galgos|apuestas carreras de
galgos en vivo|apuestas carreras de galgos nocturnas|apuestas carreras de galgos pre partido|apuestas casino|apuestas casino barcelona|apuestas casino futbol|apuestas casino gran madrid|apuestas casino gratis|apuestas casino madrid|apuestas casino online|apuestas casino online argentina|apuestas casinos|apuestas casinos
online|apuestas celta|apuestas celta barcelona|apuestas celta betis|apuestas celta eibar|apuestas celta espanyol|apuestas celta granada|apuestas celta
madrid|apuestas celta manchester|apuestas celta
real madrid|apuestas champion league|apuestas champions foro|apuestas champions hoy|apuestas champions league|apuestas champions league – pronósticos|apuestas champions league 2025|apuestas champions league hoy|apuestas champions league
pronosticos|apuestas champions league pronósticos|apuestas champions pronosticos|apuestas chelsea barcelona|apuestas chelsea betis|apuestas
chile|apuestas chile peru|apuestas chile venezuela|apuestas chile vs colombia|apuestas chile vs uruguay|apuestas
ciclismo|apuestas ciclismo en vivo|apuestas ciclismo femenino|apuestas ciclismo tour francia|apuestas ciclismo vuelta|apuestas ciclismo vuelta a españa|apuestas ciclismo vuelta españa|apuestas city madrid|apuestas
city real madrid|apuestas clasico|apuestas clasico español|apuestas clasico real madrid barcelona|apuestas clasificacion mundial|apuestas colombia|apuestas
colombia argentina|apuestas colombia brasil|apuestas colombia paraguay|apuestas colombia uruguay|apuestas
colombia vs argentina|apuestas colombia vs brasil|apuestas
combinadas|apuestas combinadas como funcionan|apuestas combinadas de
futbol|apuestas combinadas de fútbol|apuestas combinadas foro|apuestas
combinadas futbol|apuestas combinadas hoy|apuestas combinadas
mismo partido|apuestas combinadas mundial|apuestas combinadas nba|apuestas combinadas
para esta semana|apuestas combinadas para hoy|apuestas combinadas para
mañana|apuestas combinadas pronosticos|apuestas combinadas recomendadas|apuestas combinadas seguras|apuestas combinadas
seguras para hoy|apuestas combinadas seguras para mañana|apuestas como ganar|apuestas comparador|apuestas con bono de bienvenida|apuestas con dinero ficticio|apuestas con dinero real|apuestas con dinero virtual|apuestas con handicap|apuestas con handicap asiatico|apuestas con handicap baloncesto|apuestas con mas probabilidades
de ganar|apuestas con paypal|apuestas con tarjeta de credito|apuestas con tarjeta de debito|apuestas consejos|apuestas copa|apuestas copa africa|apuestas copa america|apuestas copa américa|apuestas
copa argentina|apuestas copa brasil|apuestas copa davis|apuestas
copa de europa|apuestas copa del mundo|apuestas copa del rey|apuestas copa del rey
baloncesto|apuestas copa del rey final|apuestas copa del rey futbol|apuestas copa
del rey ganador|apuestas copa del rey hoy|apuestas copa del
rey pronosticos|apuestas copa del rey pronósticos|apuestas
copa europa|apuestas copa italia|apuestas copa libertadores|apuestas copa mundial de hockey|apuestas
copa rey|apuestas copa sudamericana|apuestas corners|apuestas corners hoy|apuestas croacia argentina|apuestas
cuartos eurocopa|apuestas cuotas|apuestas cuotas altas|apuestas cuotas bajas|apuestas de
1 euro|apuestas de baloncesto|apuestas de baloncesto hoy|apuestas de baloncesto nba|apuestas de
baloncesto para hoy|apuestas de beisbol|apuestas de beisbol
para hoy|apuestas de blackjack en linea|apuestas de boxeo|apuestas de
boxeo canelo|apuestas de boxeo en las vegas|apuestas de boxeo hoy|apuestas de
boxeo online|apuestas de caballo|apuestas de caballos|apuestas de
caballos como funciona|apuestas de caballos como se juega|apuestas de caballos
en colombia|apuestas de caballos en españa|apuestas de caballos en linea|apuestas de caballos españa|apuestas de caballos ganador
y colocado|apuestas de caballos internacionales|apuestas de caballos juegos|apuestas
de caballos online|apuestas de caballos online en venezuela|apuestas de caballos por
internet|apuestas de caballos pronosticos|apuestas de caballos pronósticos|apuestas de carrera de caballos|apuestas de carreras de caballos|apuestas de carreras de caballos
online|apuestas de casino|apuestas de casino online|apuestas de casino por internet|apuestas de
champions league|apuestas de ciclismo|apuestas de colombia|apuestas de copa america|apuestas de corners|apuestas de deportes en linea|apuestas de deportes online|apuestas de dinero|apuestas de esports|apuestas de eurocopa|apuestas de europa league|apuestas
de f1|apuestas de formula 1|apuestas de futbol|apuestas de fútbol|apuestas de futbol app|apuestas de futbol argentina|apuestas de futbol colombia|apuestas de futbol en colombia|apuestas de futbol en directo|apuestas de futbol en linea|apuestas de futbol en vivo|apuestas de
futbol español|apuestas de futbol gratis|apuestas de futbol hoy|apuestas de futbol
mundial|apuestas de futbol online|apuestas de fútbol online|apuestas de futbol para hoy|apuestas
de fútbol para hoy|apuestas de futbol para hoy seguras|apuestas de futbol para mañana|apuestas de futbol peru|apuestas de futbol pronosticos|apuestas de fútbol
pronósticos|apuestas de futbol seguras|apuestas de futbol seguras para hoy|apuestas de futbol sin dinero|apuestas de galgos|apuestas de galgos como ganar|apuestas de galgos
en directo|apuestas de galgos online|apuestas de galgos trucos|apuestas de golf|apuestas de hockey|apuestas de hockey sobre hielo|apuestas de hoy|apuestas de
hoy seguras|apuestas de juego|apuestas de juegos|apuestas de juegos deportivos|apuestas de juegos
online|apuestas de la champions league|apuestas de la copa américa|apuestas de la eurocopa|apuestas de la europa
league|apuestas de la liga|apuestas de la liga bbva|apuestas de
la liga española|apuestas de la nba|apuestas de la nfl|apuestas de la ufc|apuestas
de mlb|apuestas de nba|apuestas de nba para hoy|apuestas de partidos|apuestas de partidos
de futbol|apuestas de peleas ufc|apuestas de perros en vivo|apuestas de
perros virtuales|apuestas de peru|apuestas de sistema|apuestas de sistema como funciona|apuestas de sistema explicacion|apuestas de sistema explicación|apuestas de tenis|apuestas de tenis de mesa|apuestas de tenis en directo|apuestas de tenis hoy|apuestas de tenis para hoy|apuestas de tenis pronosticos|apuestas de tenis seguras|apuestas de todo tipo|apuestas
de ufc|apuestas de ufc hoy|apuestas del boxeo|apuestas del
clasico|apuestas del clasico real madrid barca|apuestas
del dia|apuestas del día|apuestas del dia de hoy|apuestas
del dia deportivas|apuestas del dia futbol|apuestas del mundial|apuestas
del partido de hoy|apuestas del real madrid|apuestas del rey|apuestas del sistema|apuestas deporte|apuestas deportes|apuestas deportiva|apuestas deportivas|apuestas deportivas 1 euro|apuestas deportivas 10 euros gratis|apuestas deportivas 100 seguras|apuestas deportivas 1×2|apuestas deportivas android|apuestas deportivas app|apuestas deportivas apps|apuestas deportivas
argentina|apuestas deportivas argentina
futbol|apuestas deportivas argentina legal|apuestas deportivas atletico de madrid|apuestas deportivas baloncesto|apuestas deportivas barca madrid|apuestas deportivas barcelona|apuestas deportivas beisbol|apuestas deportivas bono|apuestas deportivas bono bienvenida|apuestas deportivas bono de bienvenida|apuestas deportivas bono sin deposito|apuestas deportivas bonos de bienvenida|apuestas deportivas
boxeo|apuestas deportivas caballos|apuestas deportivas calculadora|apuestas deportivas campeon liga|apuestas deportivas
casino|apuestas deportivas casino barcelona|apuestas deportivas casino online|apuestas deportivas cerca de mi|apuestas deportivas champions league|apuestas deportivas chile|apuestas deportivas ciclismo|apuestas deportivas colombia|apuestas
deportivas com|apuestas deportivas com foro|apuestas deportivas com pronosticos|apuestas deportivas combinadas|apuestas deportivas combinadas para hoy|apuestas
deportivas como se juega|apuestas deportivas comparador|apuestas deportivas con bono gratis|apuestas deportivas
con bonos gratis|apuestas deportivas con dinero ficticio|apuestas deportivas con paypal|apuestas deportivas
con puntos virtuales|apuestas deportivas consejos|apuestas deportivas consejos para ganar|apuestas deportivas copa america|apuestas deportivas copa del rey|apuestas deportivas copa libertadores|apuestas deportivas copa mundial|apuestas deportivas corners|apuestas deportivas cual es la
mejor|apuestas deportivas cuotas altas|apuestas deportivas de
baloncesto|apuestas deportivas de boxeo|apuestas deportivas de
colombia|apuestas deportivas de futbol|apuestas deportivas de nba|apuestas deportivas de nhl|apuestas
deportivas de peru|apuestas deportivas de tenis|apuestas deportivas del
dia|apuestas deportivas dinero ficticio|apuestas deportivas directo|apuestas
deportivas doble oportunidad|apuestas deportivas en argentina|apuestas deportivas en chile|apuestas deportivas en colombia|apuestas deportivas en directo|apuestas
deportivas en españa|apuestas deportivas en español|apuestas deportivas en linea|apuestas deportivas en línea|apuestas deportivas en peru|apuestas deportivas en perú|apuestas deportivas en sevilla|apuestas deportivas
en uruguay|apuestas deportivas en vivo|apuestas
deportivas es|apuestas deportivas es pronosticos|apuestas deportivas
españa|apuestas deportivas españolas|apuestas deportivas esports|apuestas deportivas estadisticas|apuestas deportivas
estrategias|apuestas deportivas estrategias seguras|apuestas deportivas eurocopa|apuestas
deportivas europa league|apuestas deportivas f1|apuestas deportivas faciles de ganar|apuestas deportivas formula 1|apuestas deportivas foro|apuestas deportivas
foro futbol|apuestas deportivas foro tenis|apuestas deportivas francia
argentina|apuestas deportivas futbol|apuestas deportivas fútbol|apuestas deportivas futbol argentino|apuestas deportivas futbol
colombia|apuestas deportivas futbol español|apuestas deportivas gana|apuestas deportivas ganadas|apuestas
deportivas ganar dinero seguro|apuestas deportivas gane|apuestas deportivas golf|apuestas deportivas
gratis|apuestas deportivas gratis con premios|apuestas deportivas gratis hoy|apuestas
deportivas gratis sin deposito|apuestas deportivas handicap|apuestas deportivas handicap asiatico|apuestas
deportivas hoy|apuestas deportivas impuestos|apuestas deportivas interior argentina|apuestas deportivas juegos olimpicos|apuestas deportivas la liga|apuestas deportivas legales|apuestas deportivas legales en colombia|apuestas deportivas libres
de impuestos|apuestas deportivas licencia españa|apuestas deportivas liga española|apuestas deportivas
listado|apuestas deportivas listado clasico|apuestas deportivas madrid|apuestas
deportivas mas seguras|apuestas deportivas mejor pagadas|apuestas deportivas mejores|apuestas deportivas mejores app|apuestas deportivas mejores casas|apuestas deportivas mejores
cuotas|apuestas deportivas mejores paginas|apuestas
deportivas mexico|apuestas deportivas méxico|apuestas deportivas
mlb|apuestas deportivas mlb hoy|apuestas deportivas multiples|apuestas
deportivas mundial|apuestas deportivas murcia|apuestas
deportivas nba|apuestas deportivas nba hoy|apuestas deportivas nfl|apuestas deportivas nhl|apuestas deportivas nuevas|apuestas deportivas ofertas|apuestas deportivas online|apuestas deportivas online argentina|apuestas deportivas online chile|apuestas deportivas
online colombia|apuestas deportivas online en colombia|apuestas deportivas online
españa|apuestas deportivas online mexico|apuestas deportivas online paypal|apuestas deportivas online peru|apuestas
deportivas online por internet|apuestas deportivas pago paypal|apuestas deportivas para ganar
dinero|apuestas deportivas para hoy|apuestas deportivas para hoy pronosticos|apuestas deportivas partido suspendido|apuestas deportivas partidos de hoy|apuestas
deportivas paypal|apuestas deportivas peru|apuestas deportivas perú|apuestas
deportivas peru vs ecuador|apuestas deportivas predicciones|apuestas deportivas
promociones|apuestas deportivas pronostico|apuestas deportivas pronóstico|apuestas deportivas pronostico hoy|apuestas deportivas pronosticos|apuestas
deportivas pronósticos|apuestas deportivas pronosticos expertos|apuestas deportivas pronosticos gratis|apuestas deportivas pronosticos nba|apuestas deportivas pronosticos tenis|apuestas deportivas que aceptan paypal|apuestas deportivas
real madrid|apuestas deportivas regalo bienvenida|apuestas deportivas resultado
exacto|apuestas deportivas resultados|apuestas deportivas rugby|apuestas
deportivas seguras|apuestas deportivas seguras foro|apuestas deportivas seguras hoy|apuestas deportivas seguras para hoy|apuestas deportivas seguras telegram|apuestas
deportivas sevilla|apuestas deportivas simulador eurocopa|apuestas
deportivas sin deposito|apuestas deportivas sin deposito
inicial|apuestas deportivas sin dinero|apuestas deportivas sin dinero real|apuestas deportivas sin registro|apuestas deportivas stake|apuestas deportivas stake 10|apuestas deportivas telegram españa|apuestas deportivas
tenis|apuestas deportivas tenis de mesa|apuestas deportivas tenis foro|apuestas deportivas tenis hoy|apuestas deportivas
tips|apuestas deportivas tipster|apuestas deportivas ufc|apuestas deportivas uruguay|apuestas
deportivas valencia|apuestas deportivas valencia barcelona|apuestas deportivas venezuela|apuestas
deportivas virtuales|apuestas deportivas y casino|apuestas deportivas y casino online|apuestas deportivas.com|apuestas deportivas.com foro|apuestas deportivas.es|apuestas deportivos pronosticos|apuestas deposito minimo 1 euro|apuestas descenso a segunda|apuestas descenso a segunda b|apuestas descenso la liga|apuestas descenso primera division|apuestas descenso segunda|apuestas dia|apuestas diarias seguras|apuestas dinero|apuestas
dinero ficticio|apuestas dinero real|apuestas dinero virtual|apuestas directas|apuestas directo|apuestas directo futbol|apuestas division de honor juvenil|apuestas dnb|apuestas doble
oportunidad|apuestas doble resultado|apuestas dobles|apuestas dobles y triples|apuestas dortmund barcelona|apuestas draft nba|apuestas draft nfl|apuestas ecuador vs argentina|apuestas ecuador
vs venezuela|apuestas egipto uruguay|apuestas el clasico|apuestas
elecciones venezuela|apuestas empate|apuestas en baloncesto|apuestas en barcelona|apuestas en beisbol|apuestas en boxeo|apuestas en caballos|apuestas en carreras de caballos|apuestas en casino|apuestas
en casino online|apuestas en casinos|apuestas en casinos
online|apuestas en chile|apuestas en ciclismo|apuestas en colombia|apuestas
en colombia de futbol|apuestas en directo|apuestas en directo futbol|apuestas en directo pronosticos|apuestas en el futbol|apuestas en el tenis|apuestas en españa|apuestas en esports|apuestas en eventos deportivos virtuales|apuestas en golf|apuestas en juegos|apuestas en la champions league|apuestas en la eurocopa|apuestas en la liga|apuestas en la nba|apuestas en la nfl|apuestas en las vegas mlb|apuestas
en las vegas nfl|apuestas en linea|apuestas en línea|apuestas en linea argentina|apuestas en linea boxeo|apuestas en linea
chile|apuestas en linea colombia|apuestas en línea de fútbol|apuestas en linea deportivas|apuestas en linea españa|apuestas
en linea estados unidos|apuestas en linea futbol|apuestas en linea mexico|apuestas en línea méxico|apuestas
en linea mundial|apuestas en linea peru|apuestas en linea usa|apuestas en los
esports|apuestas en madrid|apuestas en méxico|apuestas
en mexico online|apuestas en nba|apuestas en partidos de futbol|apuestas en partidos de futbol en vivo|apuestas
en partidos de tenis en directo|apuestas en perú|apuestas en sevilla|apuestas en sistema|apuestas en stake|apuestas en tenis|apuestas en tenis de mesa|apuestas en valencia|apuestas en vivo|apuestas en vivo argentina|apuestas en vivo casino|apuestas
en vivo futbol|apuestas en vivo fútbol|apuestas en vivo nba|apuestas en vivo peru|apuestas en vivo tenis|apuestas en vivo ufc|apuestas equipo mbappe|apuestas
equipos de futbol|apuestas españa|apuestas españa alemania|apuestas españa alemania eurocopa|apuestas españa croacia|apuestas españa eurocopa|apuestas españa francia|apuestas españa francia eurocopa|apuestas españa
gana el mundial|apuestas españa gana eurocopa|apuestas españa gana mundial|apuestas
españa georgia|apuestas españa holanda|apuestas españa inglaterra|apuestas españa inglaterra cuotas|apuestas españa inglaterra eurocopa|apuestas
españa italia|apuestas españa mundial|apuestas españa paises bajos|apuestas español|apuestas español oviedo|apuestas
espanyol barcelona|apuestas espanyol betis|apuestas espanyol villarreal|apuestas esport|apuestas esports|apuestas esports colombia|apuestas esports españa|apuestas esports fifa|apuestas esports gratis|apuestas esports lol|apuestas esports peru|apuestas esports valorant|apuestas estadisticas|apuestas estrategias|apuestas euro|apuestas euro
copa|apuestas eurocopa|apuestas eurocopa campeon|apuestas eurocopa españa|apuestas eurocopa
favoritos|apuestas eurocopa femenina|apuestas eurocopa final|apuestas eurocopa ganador|apuestas eurocopa hoy|apuestas
eurocopa sub 21|apuestas euroliga baloncesto|apuestas euroliga pronosticos|apuestas europa
league|apuestas europa league hoy|apuestas europa league pronosticos|apuestas europa league pronósticos|apuestas euros|apuestas
f1 abu dhabi|apuestas f1 bahrein|apuestas f1 canada|apuestas f1 china|apuestas f1 cuotas|apuestas f1 hoy|apuestas
f1 las vegas|apuestas f1 miami|apuestas f1 monaco|apuestas faciles de ganar|apuestas fáciles de ganar|apuestas faciles para ganar|apuestas favoritas|apuestas favorito champions|apuestas favoritos champions|apuestas favoritos
eurocopa|apuestas favoritos mundial|apuestas fc barcelona|apuestas final
champions cuotas|apuestas final champions league|apuestas final champions
peru|apuestas final copa|apuestas final copa america|apuestas final copa
de europa|apuestas final copa del rey|apuestas final copa europa|apuestas final copa libertadores|apuestas final copa rey|apuestas final de copa|apuestas final de copa del rey|apuestas final del mundial|apuestas final euro|apuestas final eurocopa|apuestas
final europa league|apuestas final libertadores|apuestas final mundial|apuestas final nba|apuestas final rugby|apuestas final uefa europa league|apuestas final.mundial|apuestas
finales de conferencia nfl|apuestas finales nba|apuestas fiorentina betis|apuestas formula|apuestas formula 1|apuestas fórmula 1|apuestas fórmula 1 pronósticos|apuestas formula uno|apuestas foro|apuestas foro nba|apuestas francia argentina|apuestas francia españa|apuestas futbol|apuestas fútbol|apuestas futbol americano|apuestas futbol
americano nfl|apuestas futbol argentina|apuestas futbol argentino|apuestas futbol champions
league|apuestas futbol chile|apuestas futbol colombia|apuestas futbol consejos|apuestas futbol en directo|apuestas fútbol en directo|apuestas futbol en vivo|apuestas fútbol en vivo|apuestas futbol españa|apuestas futbol
español|apuestas fútbol español|apuestas futbol eurocopa|apuestas futbol
femenino|apuestas futbol foro|apuestas futbol gratis|apuestas futbol hoy|apuestas fútbol hoy|apuestas futbol juegos olimpicos|apuestas futbol mexico|apuestas futbol mundial|apuestas futbol
online|apuestas futbol para hoy|apuestas futbol peru|apuestas futbol pronosticos|apuestas futbol sala|apuestas futbol telegram|apuestas futbol virtual|apuestas galgos|apuestas galgos en directo|apuestas galgos hoy|apuestas
galgos online|apuestas galgos pronosticos|apuestas galgos trucos|apuestas gana|apuestas gana colombia|apuestas gana resultados|apuestas ganadas|apuestas ganadas hoy|apuestas ganador champions league|apuestas ganador copa america|apuestas ganador
copa del rey|apuestas ganador copa del rey baloncesto|apuestas ganador copa libertadores|apuestas ganador de
la eurocopa|apuestas ganador de la liga|apuestas ganador del
mundial|apuestas ganador eurocopa|apuestas ganador europa league|apuestas ganador
f1|apuestas ganador la liga|apuestas ganador liga española|apuestas ganador mundial|apuestas
ganador mundial baloncesto|apuestas ganador mundial f1|apuestas
ganador nba|apuestas ganadores eurocopa|apuestas ganadores mundial|apuestas ganar champions|apuestas ganar eurocopa|apuestas ganar liga|apuestas ganar mundial|apuestas ganar nba|apuestas getafe valencia|apuestas ghana
uruguay|apuestas girona|apuestas girona athletic|apuestas
girona betis|apuestas girona campeon de liga|apuestas girona campeon liga|apuestas girona gana la liga|apuestas girona real madrid|apuestas
girona real sociedad|apuestas goleador eurocopa|apuestas goleadores eurocopa|apuestas goles asiaticos|apuestas
golf|apuestas golf masters|apuestas golf pga|apuestas granada barcelona|apuestas grand slam de tenis|apuestas gratis|apuestas
gratis casino|apuestas gratis con premios|apuestas gratis hoy|apuestas gratis para
hoy|apuestas gratis por registro|apuestas gratis puntos|apuestas gratis regalos|apuestas gratis sin deposito|apuestas gratis sin depósito|apuestas gratis sin ingreso|apuestas gratis sports|apuestas
gratis y ganar premios|apuestas grupo a eurocopa|apuestas grupos eurocopa|apuestas handicap|apuestas handicap asiatico|apuestas handicap baloncesto|apuestas handicap como funciona|apuestas handicap nba|apuestas handicap nfl|apuestas hipicas
online|apuestas hípicas online|apuestas hipicas venezuela|apuestas hockey|apuestas hockey hielo|apuestas hockey patines|apuestas hockey sobre hielo|apuestas holanda argentina|apuestas holanda vs argentina|apuestas hoy|apuestas hoy champions|apuestas hoy futbol|apuestas
hoy nba|apuestas hoy pronosticos|apuestas hoy seguras|apuestas impuestos|apuestas inglaterra paises bajos|apuestas inter barca|apuestas inter
barcelona|apuestas juego|apuestas juegos|apuestas juegos
en linea|apuestas juegos olimpicos|apuestas juegos
olímpicos|apuestas juegos olimpicos baloncesto|apuestas juegos online|apuestas juegos virtuales|apuestas jugador sevilla|apuestas
jugadores nba|apuestas kings league americas|apuestas la liga|apuestas la liga española|apuestas
la liga hoy|apuestas la liga santander|apuestas las vegas
mlb|apuestas las vegas nba|apuestas las vegas nfl|apuestas
league of legends mundial|apuestas legal|apuestas legales|apuestas legales
en colombia|apuestas legales en españa|apuestas legales en estados unidos|apuestas legales españa|apuestas leganes betis|apuestas
libertadores|apuestas licencia|apuestas liga 1 peru|apuestas liga argentina|apuestas liga bbva pronosticos|apuestas liga de campeones|apuestas liga de campeones de baloncesto|apuestas liga de campeones de hockey|apuestas liga españa|apuestas liga española|apuestas liga santander pronosticos|apuestas ligas de futbol|apuestas linea|apuestas linea de gol|apuestas
liverpool barcelona|apuestas liverpool real madrid|apuestas lol mundial|apuestas madrid|apuestas madrid arsenal|apuestas madrid atletico|apuestas madrid
atletico champions|apuestas madrid barca|apuestas madrid
barça|apuestas madrid barca hoy|apuestas madrid barca supercopa|apuestas madrid barcelona|apuestas madrid barsa|apuestas madrid bayern|apuestas madrid betis|apuestas
madrid borussia|apuestas madrid campeon champions|apuestas madrid
celta|apuestas madrid city|apuestas madrid dortmund|apuestas madrid gana la
liga|apuestas madrid gana liga|apuestas madrid hoy|apuestas madrid liverpool|apuestas madrid osasuna|apuestas
madrid sevilla|apuestas madrid valencia|apuestas madrid vs arsenal|apuestas
madrid vs barcelona|apuestas mallorca osasuna|apuestas mallorca real sociedad|apuestas manchester athletic|apuestas manchester city real madrid|apuestas mas faciles de
ganar|apuestas mas seguras|apuestas mas seguras para hoy|apuestas masters de golf|apuestas masters de tenis|apuestas maximo goleador eurocopa|apuestas maximo goleador mundial|apuestas mejor jugador eurocopa|apuestas mejores casinos online|apuestas mexico|apuestas méxico|apuestas mexico polonia|apuestas méxico polonia|apuestas mlb|apuestas mlb hoy|apuestas mlb las vegas|apuestas mlb para hoy|apuestas mlb pronosticos|apuestas mlb
usa|apuestas mma ufc|apuestas momios|apuestas multiples|apuestas
múltiples|apuestas multiples como funcionan|apuestas multiples el gordo|apuestas
multiples futbol|apuestas mundial|apuestas mundial 2026|apuestas mundial
baloncesto|apuestas mundial balonmano|apuestas mundial brasil|apuestas mundial campeon|apuestas mundial
ciclismo|apuestas mundial clubes|apuestas mundial de baloncesto|apuestas
mundial de ciclismo|apuestas mundial de clubes|apuestas
mundial de futbol|apuestas mundial de fútbol|apuestas mundial
de rugby|apuestas mundial f1|apuestas mundial favoritos|apuestas mundial femenino|apuestas mundial formula 1|apuestas mundial futbol|apuestas
mundial ganador|apuestas mundial lol|apuestas mundial moto gp|apuestas mundial motogp|apuestas mundial rugby|apuestas mundial sub 17|apuestas
mundiales|apuestas mundialistas|apuestas mvp eurocopa|apuestas mvp nba|apuestas mvp
nfl|apuestas nacionales de colombia|apuestas nba|apuestas nba all star|apuestas nba campeon|apuestas nba consejos|apuestas nba esta noche|apuestas nba finals|apuestas nba gratis|apuestas nba hoy|apuestas nba hoy jugadores|apuestas nba hoy pronosticos|apuestas nba para hoy|apuestas nba playoffs|apuestas nba pronosticos|apuestas nba pronósticos|apuestas nba pronosticos hoy|apuestas nba tipster|apuestas nfl|apuestas nfl hoy|apuestas nfl las vegas|apuestas nfl playoffs|apuestas nfl
pronosticos|apuestas nfl pronósticos|apuestas nfl
semana 4|apuestas nfl super bowl|apuestas nhl|apuestas nhl pronosticos|apuestas octavos
eurocopa|apuestas ofertas|apuestas online|apuestas
online argentina|apuestas online argentina legal|apuestas online bono|apuestas online bono bienvenida|apuestas online boxeo|apuestas online caballos|apuestas online carreras de caballos|apuestas online casino|apuestas online champions league|apuestas online chile|apuestas online ciclismo|apuestas online colombia|apuestas online comparativa|apuestas online
con paypal|apuestas online de caballos|apuestas online deportivas|apuestas online en argentina|apuestas online en peru|apuestas
online espana|apuestas online españa|apuestas online esports|apuestas online foro|apuestas online futbol|apuestas online futbol españa|apuestas
online golf|apuestas online gratis|apuestas online gratis sin deposito|apuestas online juegos|apuestas online
mexico|apuestas online mma|apuestas online movil|apuestas online nba|apuestas online net|apuestas online nuevas|apuestas online opiniones|apuestas online
paypal|apuestas online peru|apuestas online seguras|apuestas online
sin dinero|apuestas online sin registro|apuestas online tenis|apuestas online ufc|apuestas online uruguay|apuestas
online venezuela|apuestas open britanico golf|apuestas
osasuna athletic|apuestas osasuna barcelona|apuestas osasuna real madrid|apuestas osasuna
sevilla|apuestas osasuna valencia|apuestas over|apuestas over 2.5|apuestas over under|apuestas paginas|apuestas pago anticipado|apuestas paises bajos ecuador|apuestas paises bajos inglaterra|apuestas países bajos qatar|apuestas para boxeo|apuestas para champions league|apuestas para el
clasico|apuestas para el dia de hoy|apuestas para el mundial|apuestas
para el partido de hoy|apuestas para eurocopa|apuestas
para europa league|apuestas para futbol|apuestas para ganar|apuestas para ganar dinero|apuestas para ganar
dinero facil|apuestas para ganar en la ruleta|apuestas para ganar la champions|apuestas para ganar la eurocopa|apuestas para ganar la europa league|apuestas
para ganar la liga|apuestas para ganar siempre|apuestas para
hacer|apuestas para hoy|apuestas para hoy de futbol|apuestas para hoy europa league|apuestas para hoy futbol|apuestas para juegos|apuestas para la champions league|apuestas para la copa del rey|apuestas
para la eurocopa|apuestas para la europa league|apuestas para la final de la
eurocopa|apuestas para la nba hoy|apuestas para los partidos de hoy|apuestas para partidos de hoy|apuestas para ufc|apuestas partido|apuestas partido aplazado|apuestas
partido champions|apuestas partido colombia|apuestas partido
españa marruecos|apuestas partido mundial|apuestas partido suspendido|apuestas partidos|apuestas partidos champions league|apuestas partidos csgo|apuestas partidos
de futbol|apuestas partidos de futbol hoy|apuestas partidos de
hoy|apuestas partidos eurocopa|apuestas partidos futbol|apuestas
partidos hoy|apuestas partidos mundial|apuestas paypal|apuestas peleas de boxeo|apuestas peru|apuestas
perú|apuestas peru brasil|apuestas peru chile|apuestas peru paraguay|apuestas peru uruguay|apuestas peru vs chile|apuestas peru vs colombia|apuestas
pichichi eurocopa|apuestas plataforma|apuestas playoff|apuestas playoff ascenso|apuestas
playoff ascenso a primera|apuestas playoff nba|apuestas playoff segunda|apuestas playoff segunda b|apuestas playoffs
nba|apuestas playoffs nfl|apuestas polonia argentina|apuestas por argentina|apuestas por internet mexico|apuestas por internet para ganar dinero|apuestas por paypal|apuestas por ronda boxeo|apuestas por sistema|apuestas portugal uruguay|apuestas pre
partido|apuestas predicciones|apuestas predicciones futbol|apuestas primera division|apuestas primera division españa|apuestas promociones|apuestas pronostico|apuestas pronosticos|apuestas pronosticos deportivos|apuestas pronosticos deportivos tenis|apuestas pronosticos futbol|apuestas pronosticos gratis|apuestas pronosticos nba|apuestas pronosticos tenis|apuestas prorroga|apuestas psg barca|apuestas psg barcelona|apuestas puntos por tarjetas|apuestas puntos tarjetas|apuestas que aceptan paypal|apuestas
que es handicap|apuestas que puedes hacer con tu
novia|apuestas que siempre ganaras|apuestas que significa|apuestas quien bajara a segunda|apuestas quién bajara a segunda|apuestas quien gana el mundial|apuestas quien gana eurocopa|apuestas quien gana la champions|apuestas quien gana la
eurocopa|apuestas quien gana la liga|apuestas quien ganara el mundial|apuestas quién ganará el mundial|apuestas
quien ganara la champions|apuestas quien ganara la eurocopa|apuestas quien ganara la liga|apuestas rayo barcelona|apuestas real madrid|apuestas real
madrid arsenal|apuestas real madrid athletic|apuestas real madrid atletico|apuestas real madrid atletico champions|apuestas real madrid atletico de madrid|apuestas real
madrid atlético de madrid|apuestas real madrid
atletico madrid|apuestas real madrid barcelona|apuestas real madrid bayern|apuestas real madrid betis|apuestas
real madrid borussia|apuestas real madrid campeon champions|apuestas real madrid
celta|apuestas real madrid champions|apuestas real madrid city|apuestas real madrid girona|apuestas real madrid hoy|apuestas real
madrid liverpool|apuestas real madrid manchester city|apuestas real madrid
osasuna|apuestas real madrid real sociedad|apuestas real madrid valencia|apuestas real madrid villarreal|apuestas
real madrid vs arsenal|apuestas real madrid vs atletico|apuestas real madrid vs atlético|apuestas real
madrid vs atletico madrid|apuestas real madrid vs barcelona|apuestas real
madrid vs betis|apuestas real madrid vs sevilla|apuestas
real madrid vs valencia|apuestas real sociedad|apuestas real sociedad athletic|apuestas real sociedad barcelona|apuestas real sociedad betis|apuestas real sociedad psg|apuestas real
sociedad real madrid|apuestas real sociedad valencia|apuestas recomendadas hoy|apuestas regalo
de bienvenida|apuestas registro|apuestas resultado exacto|apuestas resultados|apuestas resultados eurocopa|apuestas retirada tenis|apuestas roma barcelona|apuestas roma sevilla|apuestas
rugby|apuestas rugby mundial|apuestas rugby world cup|apuestas ruleta seguras|apuestas
segunda|apuestas segunda b|apuestas segunda division|apuestas segunda
división|apuestas segunda division b|apuestas segunda division españa|apuestas seguras|apuestas seguras baloncesto|apuestas seguras
calculadora|apuestas seguras en la ruleta|apuestas seguras eurocopa|apuestas seguras foro|apuestas seguras futbol|apuestas
seguras futbol hoy|apuestas seguras gratis|apuestas seguras hoy|apuestas seguras hoy futbol|apuestas
seguras nba|apuestas seguras nba hoy|apuestas seguras para este fin de semana|apuestas
seguras para ganar dinero|apuestas seguras para hoy|apuestas seguras
para hoy fútbol|apuestas seguras para hoy pronósticos|apuestas seguras para
mañana|apuestas seguras ruleta|apuestas seguras telegram|apuestas seguras tenis|apuestas semifinales eurocopa|apuestas senegal paises bajos|apuestas sevilla|apuestas sevilla athletic|apuestas
sevilla atletico de madrid|apuestas sevilla barcelona|apuestas sevilla betis|apuestas sevilla campeon liga|apuestas sevilla
celta|apuestas sevilla gana la liga|apuestas sevilla girona|apuestas sevilla inter|apuestas
sevilla jugador|apuestas sevilla juventus|apuestas sevilla leganes|apuestas sevilla
madrid|apuestas sevilla manchester united|apuestas sevilla osasuna|apuestas sevilla real madrid|apuestas sevilla real
sociedad|apuestas sevilla roma|apuestas sevilla valencia|apuestas significa|apuestas simples ejemplos|apuestas simples o
combinadas|apuestas sin deposito|apuestas sin deposito
inicial|apuestas sin deposito minimo|apuestas
sin dinero|apuestas sin dinero real|apuestas sin empate|apuestas sin empate que significa|apuestas sin ingreso minimo|apuestas sin registro|apuestas sistema|apuestas sistema calculadora|apuestas sistema como funciona|apuestas sistema trixie|apuestas sociedad|apuestas sorteo copa del rey|apuestas stake|apuestas stake 10|apuestas stake
10 hoy|apuestas super bowl favorito|apuestas super rugby|apuestas supercopa españa|apuestas superliga argentina|apuestas tarjeta roja|apuestas tarjetas|apuestas tarjetas amarillas|apuestas tenis|apuestas tenis atp|apuestas tenis consejos|apuestas tenis
copa davis|apuestas tenis de mesa|apuestas tenis de mesa pronosticos|apuestas
tenis en vivo|apuestas tenis femenino|apuestas tenis hoy|apuestas tenis itf|apuestas tenis pronosticos|apuestas tenis pronósticos|apuestas tenis retirada|apuestas tenis
roland garros|apuestas tenis seguras|apuestas tenis wimbledon|apuestas tenis wta|apuestas tercera division|apuestas tercera division españa|apuestas tipos|apuestas tips|apuestas tipster|apuestas
tipster para hoy|apuestas topuria holloway cuotas|apuestas torneos de golf|apuestas torneos de
tenis|apuestas trucos|apuestas uefa champions league|apuestas uefa europa league|apuestas ufc|apuestas ufc chile|apuestas ufc como funciona|apuestas ufc hoy|apuestas ufc ilia topuria|apuestas ufc online|apuestas ufc pronósticos|apuestas
ufc telegram|apuestas ufc topuria|apuestas under over|apuestas unionistas villarreal|apuestas uruguay|apuestas
uruguay colombia|apuestas uruguay corea|apuestas uruguay vs colombia|apuestas us open golf|apuestas us open tenis|apuestas valencia|apuestas valencia barcelona|apuestas valencia betis|apuestas valencia madrid|apuestas
valencia real madrid|apuestas valladolid barcelona|apuestas valladolid valencia|apuestas
valor app|apuestas valor en directo|apuestas valor galgos|apuestas venezuela|apuestas venezuela argentina|apuestas venezuela bolivia|apuestas venezuela ecuador|apuestas villarreal|apuestas villarreal athletic|apuestas villarreal barcelona|apuestas villarreal
bayern|apuestas villarreal betis|apuestas villarreal liverpool|apuestas villarreal manchester|apuestas villarreal manchester united|apuestas villarreal vs real madrid|apuestas virtuales|apuestas virtuales colombia|apuestas virtuales futbol|apuestas virtuales sin dinero|apuestas vivo|apuestas vuelta a españa|apuestas vuelta españa|apuestas william hill partidos
de hoy|apuestas y casino|apuestas y casinos|apuestas
y juegos de azar|apuestas y pronosticos|apuestas y pronosticos de futbol|apuestas y pronosticos deportivos|apuestas y resultados|apuestas-deportivas|apuestas-deportivas.es pronosticos|arbitro nba apuestas|argentina
apuestas|argentina colombia apuestas|argentina croacia apuestas|argentina francia apuestas|argentina mexico apuestas|argentina peru apuestas|argentina uruguay apuestas|argentina vs bolivia apuestas|argentina vs chile apuestas|argentina vs colombia apuestas|argentina
vs francia apuestas|argentina vs. colombia apuestas|asi se gana en las apuestas deportivas|asiatico apuestas|asiatico en apuestas|asiaticos apuestas|athletic barcelona apuestas|athletic manchester united
apuestas|athletic osasuna apuestas|athletic real madrid apuestas|atletico
barcelona apuestas|atletico de madrid apuestas|atlético de madrid apuestas|atletico de madrid real madrid
apuestas|atletico de madrid vs barcelona apuestas|atletico
madrid real madrid apuestas|atletico madrid vs real madrid
apuestas|atletico real madrid apuestas|atletico vs real madrid apuestas|avisador de cuotas apuestas|bajada de cuotas apuestas|baloncesto apuestas|barbastro barcelona apuestas|barca apuestas|barca bayern apuestas|barca
inter apuestas|barca madrid apuestas|barça madrid apuestas|barca
vs atletico apuestas|barca vs madrid apuestas|barca vs real madrid apuestas|barcelona – real madrid apuestas|barcelona apuestas|barcelona atletico apuestas|barcelona atletico de
madrid apuestas|barcelona atletico madrid apuestas|barcelona betis apuestas|barcelona casa de apuestas|barcelona inter
apuestas|barcelona psg apuestas|barcelona real madrid apuestas|barcelona real sociedad apuestas|barcelona sevilla apuestas|barcelona valencia apuestas|barcelona vs athletic bilbao apuestas|barcelona vs atlético
madrid apuestas|barcelona vs betis apuestas|barcelona vs celta de vigo
apuestas|barcelona vs espanyol apuestas|barcelona
vs girona apuestas|barcelona vs madrid apuestas|barcelona
vs real madrid apuestas|barcelona vs real sociedad apuestas|barcelona vs sevilla apuestas|barcelona vs villarreal apuestas|base
de datos cuotas apuestas deportivas|bayern real madrid apuestas|beisbol apuestas|best america
apuestas|bet apuestas chile|bet apuestas en vivo|betis – chelsea
apuestas|betis apuestas|betis barcelona apuestas|betis chelsea apuestas|betis madrid apuestas|betis sevilla
apuestas|betsson tu sitio de apuestas online|blog apuestas baloncesto|blog apuestas ciclismo|blog apuestas nba|blog apuestas
tenis|blog de apuestas de tenis|bono apuestas|bono apuestas deportivas|bono apuestas deportivas sin deposito|bono apuestas gratis|bono apuestas gratis sin deposito|bono apuestas sin deposito|bono bienvenida apuestas|bono bienvenida apuestas deportivas|bono bienvenida apuestas españa|bono bienvenida apuestas sin deposito|bono bienvenida apuestas sin depósito|bono
bienvenida casa apuestas|bono bienvenida casa de apuestas|bono bienvenida marca apuestas|bono casa apuestas|bono casa
de apuestas|bono casa de apuestas sin ingreso|bono casas de apuestas|bono
de apuestas|bono de apuestas gratis sin deposito|bono de bienvenida apuestas|bono de bienvenida apuestas deportivas|bono de bienvenida casa de apuestas|bono de bienvenida casas de apuestas|bono
de casas de apuestas|bono de registro apuestas|bono de registro apuestas deportivas|bono de registro casa de apuestas|bono gratis apuestas|bono marca apuestas|bono por registro
apuestas|bono por registro apuestas deportivas|bono por registro casa de apuestas|bono registro apuestas|bono sin deposito apuestas|bono sin depósito apuestas|bono sin deposito apuestas deportivas|bono sin depósito apuestas deportivas|bono sin deposito casa de apuestas|bono sin deposito
marca apuestas|bono sin ingreso apuestas|bono sin ingreso apuestas deportivas|bonos
apuestas|bonos apuestas colombia|bonos apuestas deportivas|bonos
apuestas deportivas sin deposito|bonos apuestas gratis|bonos apuestas sin deposito|bonos apuestas sin depósito|bonos bienvenida apuestas|bonos bienvenida casas
apuestas|bonos bienvenida casas de apuestas|bonos casa
de apuestas|bonos casas apuestas|bonos casas de apuestas|bonos casas
de apuestas colombia|bonos casas de apuestas deportivas|bonos casas de apuestas españa|bonos casas de apuestas nuevas|bonos casas de
apuestas sin deposito|bonos casas de apuestas sin depósito|bonos de apuestas|bonos de apuestas deportivas|bonos de apuestas gratis|bonos de apuestas sin deposito|bonos
de bienvenida apuestas|bonos de bienvenida apuestas deportivas|bonos de
bienvenida casa de apuestas|bonos de bienvenida casas
de apuestas|bonos de bienvenida de casas de apuestas|bonos
de bienvenida en casas de apuestas|bonos de casas de apuestas|bonos de casas de apuestas sin deposito|bonos en casa de apuestas|bonos en casas de apuestas sin deposito|bonos gratis apuestas|bonos gratis apuestas deportivas|bonos gratis casas de apuestas|bonos gratis sin deposito
apuestas|bonos paginas de apuestas|bonos registro
casas de apuestas|bonos sin deposito apuestas|bonos sin depósito
apuestas|bonos sin deposito apuestas deportivas|bonos sin deposito casas
de apuestas|bot de apuestas deportivas gratis|boxeo apuestas|brasil
colombia apuestas|brasil peru apuestas|brasil vs colombia apuestas|buenas apuestas para hoy|buscador cuotas apuestas|buscador de apuestas seguras|buscador de cuotas apuestas|buscador de cuotas de apuestas|buscar apuestas
seguras|caballos apuestas|calculador de apuestas|calculador
de cuotas apuestas|calculadora apuestas|calculadora apuestas combinadas|calculadora apuestas de sistema|calculadora apuestas deportivas|calculadora apuestas deportivas seguras|calculadora apuestas multiples|calculadora apuestas segura|calculadora apuestas
seguras|calculadora apuestas sistema|calculadora apuestas yankee|calculadora arbitraje
apuestas|calculadora cubrir apuestas|calculadora
cuotas apuestas|calculadora de apuestas|calculadora
de apuestas combinadas|calculadora de apuestas de futbol|calculadora de apuestas de sistema|calculadora de apuestas deportivas|calculadora de apuestas multiples|calculadora de apuestas seguras|calculadora de apuestas sistema|calculadora de apuestas surebets|calculadora de arbitraje apuestas|calculadora de cuotas apuestas|calculadora de cuotas de apuestas|calculadora para apuestas deportivas|calculadora poisson apuestas|calculadora poisson apuestas deportivas|calculadora poisson para apuestas|calculadora scalping apuestas deportivas|calculadora sistema apuestas|calculadora stake apuestas|calculadora trading apuestas|calcular apuestas|calcular apuestas deportivas|calcular apuestas
futbol|calcular apuestas sistema|calcular cuotas apuestas|calcular cuotas apuestas combinadas|calcular cuotas apuestas deportivas|calcular cuotas de apuestas|calcular ganancias apuestas
deportivas|calcular momios apuestas|calcular probabilidad cuota apuestas|calcular stake
apuestas|calcular unidades apuestas|calcular yield apuestas|calculo de
apuestas|calculo de apuestas deportivas|cambio de cuotas apuestas|campeon champions apuestas|campeon eurocopa apuestas|campeon liga apuestas|campeon nba apuestas|canales de apuestas gratis|carrera de caballos apuestas|carrera de caballos apuestas juego|carrera de caballos con apuestas|carrera de galgos apuestas|carreras de caballos apuestas|carreras de caballos
apuestas online|carreras de caballos con apuestas|carreras
de caballos juegos de apuestas|carreras de galgos apuestas|carreras
de galgos apuestas online|carreras de galgos apuestas trucos|carreras galgos apuestas|casa apuestas argentina|casa apuestas atletico de
madrid|casa apuestas barcelona|casa apuestas betis|casa apuestas bono bienvenida|casa apuestas bono gratis|casa apuestas bono sin deposito|casa apuestas cerca de
mi|casa apuestas chile|casa apuestas colombia|casa
apuestas con mejores cuotas|casa apuestas deportivas|casa apuestas españa|casa apuestas española|casa
apuestas eurocopa|casa apuestas futbol|casa
apuestas mejores cuotas|casa apuestas mundial|casa apuestas nueva|casa apuestas nuevas|casa apuestas
online|casa apuestas peru|casa apuestas valencia|casa de apuestas|casa de apuestas
10 euros gratis|casa de apuestas argentina|casa de
apuestas atletico de madrid|casa de apuestas baloncesto|casa de apuestas barcelona|casa de apuestas
beisbol|casa de apuestas betis|casa de apuestas bono|casa de apuestas bono bienvenida|casa
de apuestas bono de bienvenida|casa de apuestas bono gratis|casa de apuestas bono
por registro|casa de apuestas bono sin deposito|casa de
apuestas boxeo|casa de apuestas caballos|casa de apuestas carreras de caballos|casa de apuestas cerca de mi|casa de apuestas cerca de mí|casa de apuestas champions league|casa de apuestas chile|casa de apuestas
ciclismo|casa de apuestas colombia|casa de apuestas con bono de bienvenida|casa de apuestas con bono sin deposito|casa de apuestas con cuotas mas altas|casa de apuestas con esports|casa de apuestas con las mejores cuotas|casa de apuestas con licencia en españa|casa de apuestas
con mejores cuotas|casa de apuestas con pago anticipado|casa de apuestas con paypal|casa de apuestas copa america|casa de apuestas
de caballos|casa de apuestas de colombia|casa de apuestas
de españa|casa de apuestas de futbol|casa de apuestas de fútbol|casa de apuestas de
futbol peru|casa de apuestas de peru|casa de apuestas del madrid|casa de apuestas del real madrid|casa
de apuestas deportivas|casa de apuestas deportivas cerca de mi|casa de
apuestas deportivas en argentina|casa de apuestas deportivas en chile|casa de apuestas deportivas en colombia|casa de apuestas deportivas en españa|casa de apuestas deportivas en madrid|casa de apuestas
deportivas españa|casa de apuestas deportivas españolas|casa de apuestas deportivas madrid|casa de apuestas deportivas mexico|casa de apuestas
deportivas online|casa de apuestas deportivas peru|casa
de apuestas deposito 5 euros|casa de apuestas deposito minimo|casa de apuestas deposito minimo 1 euro|casa de apuestas
depósito mínimo 1 euro|casa de apuestas en españa|casa de apuestas en linea|casa de apuestas en madrid|casa de apuestas
en perú|casa de apuestas en vivo|casa de apuestas españa|casa de
apuestas españa inglaterra|casa de apuestas española|casa de apuestas españolas|casa de
apuestas esports|casa de apuestas eurocopa|casa de apuestas europa
league|casa de apuestas f1|casa de apuestas formula 1|casa de apuestas futbol|casa de
apuestas ingreso minimo|casa de apuestas ingreso minimo 1 euro|casa
de apuestas ingreso mínimo 1 euro|casa de apuestas legales|casa de apuestas legales en colombia|casa de apuestas legales en españa|casa de apuestas libertadores|casa de
apuestas liga española|casa de apuestas madrid|casa de apuestas mas segura|casa de apuestas mejores|casa
de apuestas méxico|casa de apuestas minimo 5 euros|casa de apuestas mlb|casa de apuestas mundial|casa de apuestas nba|casa de apuestas nfl|casa de apuestas nueva|casa de
apuestas nuevas|casa de apuestas oficial del real madrid|casa de apuestas oficial real madrid|casa de apuestas online|casa de apuestas online argentina|casa de apuestas online chile|casa de apuestas online españa|casa de apuestas
online mexico|casa de apuestas online paraguay|casa de apuestas online peru|casa de apuestas online usa|casa de apuestas online venezuela|casa de apuestas pago anticipado|casa
de apuestas para boxeo|casa de apuestas para ufc|casa de apuestas peru|casa de apuestas perú|casa de apuestas peru online|casa de apuestas por
paypal|casa de apuestas promociones|casa de apuestas que regalan dinero|casa de apuestas real
madrid|casa de apuestas regalo de bienvenida|casa de apuestas sevilla|casa
de apuestas sin dinero|casa de apuestas sin ingreso minimo|casa de apuestas sin licencia en españa|casa de apuestas sin minimo de ingreso|casa de apuestas stake|casa de apuestas tenis|casa de apuestas ufc|casa
de apuestas valencia|casa de apuestas venezuela|casa
de apuestas virtuales|casa de apuestas vive la suerte|casa oficial de apuestas
del real madrid|casas apuestas asiaticas|casas apuestas bono sin deposito|casas apuestas bonos sin deposito|casas apuestas
caballos|casas apuestas chile|casas apuestas ciclismo|casas apuestas con licencia|casas apuestas con licencia en españa|casas apuestas deportivas|casas apuestas deportivas colombia|casas apuestas deportivas españa|casas apuestas deportivas españolas|casas apuestas deportivas nuevas|casas apuestas
españa|casas apuestas españolas|casas apuestas esports|casas apuestas eurocopa|casas apuestas
golf|casas apuestas ingreso minimo 5 euros|casas apuestas legales|casas apuestas legales españa|casas apuestas licencia|casas apuestas licencia españa|casas apuestas mexico|casas apuestas mundial|casas apuestas nba|casas apuestas nuevas|casas apuestas nuevas españa|casas apuestas ofertas|casas apuestas online|casas apuestas paypal|casas apuestas peru|casas apuestas sin licencia|casas
apuestas tenis|casas asiaticas apuestas|casas de apuestas|casas
de apuestas 5 euros|casas de apuestas app|casas de apuestas argentinas|casas de apuestas asiaticas|casas de apuestas
baloncesto|casas de apuestas barcelona|casas de apuestas bono
bienvenida|casas de apuestas bono de bienvenida|casas de apuestas bono por registro|casas de apuestas bono sin deposito|casas de apuestas bono sin ingreso|casas de apuestas bonos|casas de apuestas
bonos de bienvenida|casas de apuestas bonos gratis|casas de apuestas
bonos sin deposito|casas de apuestas boxeo|casas de apuestas caballos|casas de apuestas carreras de caballos|casas de
apuestas casino|casas de apuestas casino online|casas de apuestas cerca de mi|casas
de apuestas champions league|casas de apuestas chile|casas de apuestas ciclismo|casas de
apuestas colombia|casas de apuestas com|casas de apuestas con app|casas
de apuestas con apuestas gratis|casas de apuestas con bono|casas de
apuestas con bono de bienvenida|casas de apuestas con bono de registro|casas de apuestas con bono por registro|casas de apuestas con bono
sin deposito|casas de apuestas con bonos|casas de apuestas
con bonos gratis|casas de apuestas con bonos sin deposito|casas
de apuestas con deposito minimo|casas de apuestas con esports|casas de apuestas con handicap asiatico|casas de apuestas con licencia|casas
de apuestas con licencia en españa|casas de apuestas con licencia
españa|casas de apuestas con licencia española|casas de apuestas con mejores cuotas|casas
de apuestas con pago anticipado|casas de apuestas con paypal|casas de apuestas con paypal en perú|casas de apuestas
con promociones|casas de apuestas con ruleta en vivo|casas de apuestas copa del rey|casas de apuestas de caballos|casas de apuestas de españa|casas de apuestas de futbol|casas de apuestas de fútbol|casas de apuestas de peru|casas de apuestas deportivas|casas de apuestas deportivas
asiaticas|casas de apuestas deportivas colombia|casas de apuestas deportivas comparativa|casas de apuestas
deportivas con paypal|casas de apuestas deportivas en chile|casas de apuestas deportivas en españa|casas
de apuestas deportivas en linea|casas de apuestas deportivas en madrid|casas de apuestas deportivas en mexico|casas de apuestas deportivas en peru|casas de
apuestas deportivas en sevilla|casas de apuestas deportivas en valencia|casas de apuestas deportivas españa|casas de apuestas deportivas españolas|casas de
apuestas deportivas legales|casas de apuestas deportivas madrid|casas de apuestas deportivas
mexico|casas de apuestas deportivas nuevas|casas de apuestas deportivas
online|casas de apuestas deportivas peru|casas de apuestas deportivas perú|casas de apuestas deposito minimo 1 euro|casas de apuestas depósito mínimo 1 euro|casas
de apuestas dinero gratis|casas de apuestas en argentina|casas de apuestas en barcelona|casas de apuestas
en chile|casas de apuestas en colombia|casas de apuestas en españa|casas de apuestas en españa
online|casas de apuestas en linea|casas de apuestas en madrid|casas de
apuestas en méxico|casas de apuestas en peru|casas de apuestas en perú|casas de apuestas en sevilla|casas de apuestas en uruguay|casas de
apuestas en valencia|casas de apuestas en venezuela|casas de apuestas equipos de
futbol|casas de apuestas españa|casas de apuestas españa alemania|casas de apuestas españa
inglaterra|casas de apuestas españa licencia|casas de apuestas españa nuevas|casas de apuestas españa online|casas de apuestas española|casas
de apuestas españolas|casas de apuestas españolas con licencia|casas de apuestas españolas online|casas de
apuestas esports|casas de apuestas eurocopa|casas
de apuestas eurocopa 2024|casas de apuestas europa league|casas de apuestas f1|casas de apuestas fisicas en barcelona|casas de
apuestas fisicas en españa|casas de apuestas formula 1|casas
de apuestas fuera de españa|casas de apuestas futbol|casas
de apuestas fútbol|casas de apuestas futbol españa|casas de apuestas
ganador eurocopa|casas de apuestas gratis|casas de apuestas ingreso minimo|casas de
apuestas ingreso minimo 1 euro|casas de apuestas ingreso minimo 5 euros|casas de
apuestas inter barcelona|casas de apuestas legales|casas de apuestas legales en colombia|casas de apuestas legales en españa|casas
de apuestas legales en mexico|casas de apuestas legales españa|casas de apuestas legales mx|casas de apuestas licencia|casas de apuestas licencia españa|casas de apuestas lista|casas de apuestas madrid|casas de apuestas mas
seguras|casas de apuestas mejores bonos|casas de apuestas mejores cuotas|casas
de apuestas mexico|casas de apuestas méxico|casas de apuestas minimo 5
euros|casas de apuestas mlb|casas de apuestas mundial|casas de apuestas mundial baloncesto|casas de apuestas mundiales|casas de apuestas nba|casas de apuestas no reguladas en españa|casas de apuestas nueva ley|casas de apuestas nuevas|casas de apuestas
nuevas en colombia|casas de apuestas nuevas en españa|casas
de apuestas nuevas españa|casas de apuestas ofertas|casas de apuestas
online|casas de apuestas online argentina|casas de apuestas online
colombia|casas de apuestas online deportivas|casas de
apuestas online ecuador|casas de apuestas online en argentina|casas de apuestas online en chile|casas
de apuestas online en colombia|casas de apuestas online
en españa|casas de apuestas online en mexico|casas de apuestas online españa|casas de apuestas
online mas fiables|casas de apuestas online mexico|casas de apuestas online nuevas|casas de apuestas online peru|casas de apuestas online usa|casas de apuestas online venezuela|casas
de apuestas pago paypal|casas de apuestas para ufc|casas de apuestas paypal|casas de apuestas
peru bono sin deposito|casas de apuestas presenciales en españa|casas de apuestas
promociones|
(10 euros gratis apuestas|10 mejores casas de apuestas|10 trucos para ganar apuestas|15 euros
gratis marca apuestas|1×2 apuestas|1×2 apuestas deportivas|1×2
apuestas que significa|1×2 en apuestas|1×2 en apuestas que significa|1×2 que significa en apuestas|5 euros gratis apuestas|9 apuestas que siempre ganaras|a partir de
cuanto se declara apuestas|actividades de juegos de azar y apuestas|ad apuestas deportivas|aleksandre topuria
ufc apuestas|algoritmo para ganar apuestas deportivas|america apuestas|análisis nba apuestas|aplicacion android apuestas deportivas|aplicacion apuestas deportivas|aplicacion apuestas deportivas android|aplicación de apuestas online|aplicacion para hacer apuestas|aplicacion para hacer apuestas de futbol|aplicación para hacer apuestas de fútbol|aplicaciones apuestas deportivas android|aplicaciones
apuestas deportivas gratis|aplicaciones de apuestas android|aplicaciones de apuestas de fútbol|aplicaciones de apuestas deportivas|aplicaciones de apuestas deportivas peru|aplicaciones de apuestas deportivas perú|aplicaciones de apuestas
en colombia|aplicaciones de apuestas gratis|aplicaciones de
apuestas online|aplicaciones de apuestas seguras|aplicaciones de apuestas sin dinero|aplicaciones para hacer
apuestas|apostar seguro apuestas deportivas|app android apuestas
deportivas|app apuestas|app apuestas android|app apuestas de
futbol|app apuestas deportivas|app apuestas deportivas android|app apuestas deportivas
argentina|app apuestas deportivas colombia|app apuestas deportivas ecuador|app apuestas deportivas españa|app apuestas deportivas gratis|app
apuestas entre amigos|app apuestas futbol|app apuestas gratis|app apuestas sin dinero|app casa de apuestas|app casas de apuestas|app control
apuestas|app de apuestas|app de apuestas android|app de
apuestas casino|app de apuestas colombia|app de apuestas con bono de bienvenida|app
de apuestas de futbol|app de apuestas deportivas|app de apuestas
deportivas android|app de apuestas deportivas argentina|app de apuestas deportivas
colombia|app de apuestas deportivas en españa|app de apuestas
deportivas peru|app de apuestas deportivas perú|app de apuestas deportivas
sin dinero|app de apuestas ecuador|app de apuestas en colombia|app
de apuestas en españa|app de apuestas en venezuela|app de apuestas futbol|app de
apuestas gratis|app de apuestas online|app de apuestas para android|app de apuestas
para ganar dinero|app de apuestas peru|app de apuestas reales|app
de casas de apuestas|app marca apuestas android|app moviles
de apuestas|app para apuestas|app para apuestas de futbol|app
para apuestas deportivas|app para apuestas deportivas en español|app para
ganar apuestas deportivas|app para hacer apuestas|app para hacer apuestas deportivas|app para hacer apuestas entre amigos|app para llevar control de apuestas|app pronosticos apuestas deportivas|app versus apuestas|apps apuestas
mundial|apps de apuestas|apps de apuestas con bono de bienvenida|apps de apuestas de futbol|apps
de apuestas deportivas peru|apps de apuestas mexico|apps para apuestas|aprender a hacer apuestas
deportivas|aprender hacer apuestas deportivas|apuesta del dia
apuestas deportivas|apuestas 10 euros gratis|apuestas 100 seguras|apuestas 1×2|apuestas 1X2|apuestas
2 division|apuestas 3 division|apuestas a caballos|apuestas a
carreras de caballos|apuestas a colombia|apuestas a
corners|apuestas a ganar|apuestas a jugadores nba|apuestas a la baja|apuestas
a la nfl|apuestas al barcelona|apuestas al dia|apuestas
al empate|apuestas al mundial|apuestas al tenis wta|apuestas alaves barcelona|apuestas
alcaraz hoy|apuestas alemania españa|apuestas alonso campeon del mundo|apuestas altas
y bajas|apuestas altas y bajas nfl|apuestas ambos equipos marcan|apuestas
america|apuestas android|apuestas anillo nba|apuestas
antes del mundial|apuestas anticipadas|apuestas anticipadas nba|apuestas apps|apuestas arabia argentina|apuestas argentina|apuestas argentina campeon del mundo|apuestas argentina canada|apuestas argentina colombia|apuestas argentina croacia|apuestas argentina españa|apuestas argentina francia|apuestas argentina francia cuanto paga|apuestas argentina francia mundial|apuestas argentina gana el mundial|apuestas argentina gana mundial|apuestas argentina
holanda|apuestas argentina mexico|apuestas argentina méxico|apuestas argentina mundial|apuestas argentina online|apuestas argentina paises bajos|apuestas argentina
polonia|apuestas argentina uruguay|apuestas argentina vs
australia|apuestas argentina vs colombia|apuestas argentina vs francia|apuestas argentina vs peru|apuestas argentinas|apuestas
arsenal real madrid|apuestas ascenso a primera division|apuestas ascenso a segunda|apuestas asiaticas|apuestas
asiatico|apuestas athletic|apuestas athletic atletico|apuestas athletic barça|apuestas athletic barcelona|apuestas athletic betis|apuestas athletic manchester|apuestas athletic manchester
united|apuestas athletic osasuna|apuestas athletic real|apuestas athletic real madrid|apuestas athletic real sociedad|apuestas athletic real sociedad final|apuestas athletic roma|apuestas athletic sevilla|apuestas athletic valencia|apuestas atletico|apuestas atletico barcelona|apuestas atletico barsa|apuestas atletico campeon champions|apuestas atletico campeon de liga|apuestas atlético copenhague|apuestas atletico de madrid|apuestas atlético de madrid|apuestas atletico de madrid barcelona|apuestas atletico de madrid gana
la liga|apuestas atletico de madrid real madrid|apuestas atlético de madrid real madrid|apuestas atletico de madrid vs barcelona|apuestas atletico madrid|apuestas atletico madrid real madrid|apuestas atletico madrid vs barcelona|apuestas atletico real madrid|apuestas atletico real madrid champions|apuestas atletismo|apuestas bajas|apuestas baloncesto|apuestas baloncesto acb|apuestas baloncesto handicap|apuestas baloncesto hoy|apuestas baloncesto juegos olimpicos|apuestas baloncesto nba|apuestas baloncesto pronostico|apuestas baloncesto pronósticos|apuestas
baloncesto prorroga|apuestas barca|apuestas barca athletic|apuestas barca atletico|apuestas barca bayern|apuestas barca bayern munich|apuestas barca girona|apuestas barca hoy|apuestas barça hoy|apuestas barca
inter|apuestas barca juventus|apuestas barca madrid|apuestas barça madrid|apuestas barca real madrid|apuestas barca vs juve|apuestas barca vs madrid|apuestas barca vs psg|apuestas barcelona|apuestas barcelona alaves|apuestas barcelona athletic|apuestas barcelona atletico|apuestas barcelona atletico de madrid|apuestas barcelona atlético de madrid|apuestas barcelona
atletico madrid|apuestas barcelona bayern|apuestas barcelona betis|apuestas barcelona campeon de liga|apuestas barcelona celta|apuestas barcelona
espanyol|apuestas barcelona gana la champions|apuestas barcelona girona|apuestas barcelona granada|apuestas barcelona hoy|apuestas barcelona inter|apuestas barcelona madrid|apuestas barcelona osasuna|apuestas barcelona psg|apuestas barcelona real madrid|apuestas barcelona real sociedad|apuestas barcelona sevilla|apuestas barcelona valencia|apuestas barcelona villarreal|apuestas
barcelona vs atletico madrid|apuestas barcelona vs
madrid|apuestas barcelona vs real madrid|apuestas barsa madrid|apuestas basket hoy|apuestas bayern barcelona|apuestas bayern vs barcelona|apuestas beisbol|apuestas béisbol|apuestas beisbol mlb|apuestas beisbol pronosticos|apuestas beisbol venezolano|apuestas betis|apuestas betis – chelsea|apuestas betis barcelona|apuestas
betis chelsea|apuestas betis fiorentina|apuestas betis girona|apuestas betis madrid|apuestas betis
mallorca|apuestas betis real madrid|apuestas betis real sociedad|apuestas
betis sevilla|apuestas betis valencia|apuestas betis valladolid|apuestas betis vs valencia|apuestas betplay hoy
colombia|apuestas betsson peru|apuestas bienvenida|apuestas billar online|apuestas bolivia vs
colombia|apuestas bono|apuestas bono bienvenida|apuestas bono de bienvenida|apuestas
bono de bienvenida sin deposito|apuestas bono gratis|apuestas bono sin deposito|apuestas bonos sin deposito|apuestas borussia real madrid|apuestas boxeo|apuestas boxeo de campeonato|apuestas boxeo españa|apuestas boxeo español|apuestas boxeo femenino olimpiadas|apuestas boxeo hoy|apuestas boxeo online|apuestas
brasil colombia|apuestas brasil peru|apuestas brasil uruguay|apuestas
brasil vs colombia|apuestas brasil vs peru|apuestas caballos|apuestas caballos colocado|apuestas caballos españa|apuestas
caballos hipodromo|apuestas caballos hoy|apuestas caballos madrid|apuestas
caballos online|apuestas caballos sanlucar de barrameda|apuestas caballos zarzuela|apuestas calculador|apuestas campeon|apuestas campeon champions|apuestas
campeón champions|apuestas campeon champions 2025|apuestas campeon champions league|apuestas campeon conference league|apuestas campeon copa america|apuestas campeon copa del rey|apuestas campeon de champions|apuestas campeon de la champions|apuestas campeon de liga|apuestas campeon del mundo|apuestas campeon eurocopa|apuestas campeón eurocopa|apuestas campeon europa league|apuestas campeon f1|apuestas campeon f1 2025|apuestas campeon formula 1|apuestas campeon libertadores|apuestas
campeon liga|apuestas campeon liga bbva|apuestas
campeon liga española|apuestas campeon liga santander|apuestas campeon motogp 2025|apuestas campeon mundial|apuestas campeón mundial|apuestas campeon mundial baloncesto|apuestas campeon nba|apuestas campeón nba|apuestas campeon premier|apuestas campeon premier league|apuestas campeon roland garros|apuestas campeonato f1|apuestas campeonatos
de futbol|apuestas carrera de caballos|apuestas carrera de caballos hoy|apuestas carrera de caballos nocturnas|apuestas carrera de galgos fin de semana|apuestas carrera de galgos hoy|apuestas carrera de galgos nocturnas|apuestas carreras caballos|apuestas
carreras caballos sanlucar|apuestas carreras de caballos|apuestas carreras de caballos en directo|apuestas carreras de caballos
en vivo|apuestas carreras de caballos españa|apuestas carreras de caballos hoy|apuestas carreras de caballos
nacionales|apuestas carreras de caballos nocturnas|apuestas carreras de caballos
online|apuestas carreras de caballos sanlucar|apuestas carreras
de caballos sanlúcar|apuestas carreras de galgos|apuestas carreras de galgos en vivo|apuestas carreras de galgos nocturnas|apuestas carreras de galgos pre partido|apuestas casino|apuestas casino
barcelona|apuestas casino futbol|apuestas casino gran madrid|apuestas casino gratis|apuestas casino madrid|apuestas casino
online|apuestas casino online argentina|apuestas casinos|apuestas
casinos online|apuestas celta|apuestas celta barcelona|apuestas celta betis|apuestas celta
eibar|apuestas celta espanyol|apuestas celta granada|apuestas celta madrid|apuestas celta manchester|apuestas celta real madrid|apuestas champion league|apuestas champions foro|apuestas
champions hoy|apuestas champions league|apuestas champions
league – pronósticos|apuestas champions league
2025|apuestas champions league hoy|apuestas champions league pronosticos|apuestas
champions league pronósticos|apuestas champions pronosticos|apuestas chelsea barcelona|apuestas chelsea betis|apuestas chile|apuestas chile peru|apuestas chile venezuela|apuestas chile vs colombia|apuestas chile vs uruguay|apuestas ciclismo|apuestas ciclismo en vivo|apuestas ciclismo femenino|apuestas ciclismo tour francia|apuestas ciclismo vuelta|apuestas ciclismo vuelta a españa|apuestas ciclismo
vuelta españa|apuestas city madrid|apuestas city real madrid|apuestas clasico|apuestas clasico español|apuestas clasico
real madrid barcelona|apuestas clasificacion mundial|apuestas colombia|apuestas
colombia argentina|apuestas colombia brasil|apuestas colombia paraguay|apuestas colombia
uruguay|apuestas colombia vs argentina|apuestas colombia vs brasil|apuestas combinadas|apuestas combinadas como funcionan|apuestas combinadas de futbol|apuestas combinadas
de fútbol|apuestas combinadas foro|apuestas combinadas
futbol|apuestas combinadas hoy|apuestas combinadas mismo partido|apuestas
combinadas mundial|apuestas combinadas nba|apuestas combinadas para esta semana|apuestas combinadas para hoy|apuestas combinadas para mañana|apuestas combinadas
pronosticos|apuestas combinadas recomendadas|apuestas combinadas seguras|apuestas combinadas seguras para hoy|apuestas combinadas seguras para mañana|apuestas como ganar|apuestas
comparador|apuestas con bono de bienvenida|apuestas con dinero ficticio|apuestas con dinero real|apuestas con dinero virtual|apuestas con handicap|apuestas con handicap asiatico|apuestas con handicap baloncesto|apuestas con mas probabilidades
de ganar|apuestas con paypal|apuestas con tarjeta de credito|apuestas con tarjeta de
debito|apuestas consejos|apuestas copa|apuestas copa africa|apuestas
copa america|apuestas copa américa|apuestas copa argentina|apuestas copa
brasil|apuestas copa davis|apuestas copa de europa|apuestas copa del mundo|apuestas copa del rey|apuestas copa
del rey baloncesto|apuestas copa del rey final|apuestas copa del rey futbol|apuestas copa del rey ganador|apuestas copa del rey hoy|apuestas copa del rey pronosticos|apuestas copa del rey pronósticos|apuestas copa europa|apuestas copa italia|apuestas copa libertadores|apuestas copa mundial de hockey|apuestas copa rey|apuestas copa sudamericana|apuestas corners|apuestas corners hoy|apuestas croacia argentina|apuestas cuartos
eurocopa|apuestas cuotas|apuestas cuotas altas|apuestas cuotas bajas|apuestas de 1 euro|apuestas de baloncesto|apuestas de baloncesto hoy|apuestas de baloncesto nba|apuestas de baloncesto para hoy|apuestas de beisbol|apuestas de beisbol para hoy|apuestas de blackjack en linea|apuestas de boxeo|apuestas de boxeo canelo|apuestas de boxeo en las vegas|apuestas de boxeo hoy|apuestas de boxeo online|apuestas de caballo|apuestas de caballos|apuestas
de caballos como funciona|apuestas de caballos como se juega|apuestas
de caballos en colombia|apuestas de caballos en españa|apuestas de caballos en linea|apuestas de caballos españa|apuestas de caballos
ganador y colocado|apuestas de caballos internacionales|apuestas de caballos juegos|apuestas de caballos online|apuestas de caballos
online en venezuela|apuestas de caballos por internet|apuestas de caballos pronosticos|apuestas de caballos pronósticos|apuestas de carrera de caballos|apuestas de carreras
de caballos|apuestas de carreras de caballos online|apuestas
de casino|apuestas de casino online|apuestas de casino por internet|apuestas de champions league|apuestas de ciclismo|apuestas de colombia|apuestas de copa america|apuestas
de corners|apuestas de deportes en linea|apuestas de deportes online|apuestas de dinero|apuestas de esports|apuestas de eurocopa|apuestas
de europa league|apuestas de f1|apuestas de formula 1|apuestas de futbol|apuestas de fútbol|apuestas
de futbol app|apuestas de futbol argentina|apuestas de futbol colombia|apuestas de futbol en colombia|apuestas de
futbol en directo|apuestas de futbol en linea|apuestas de futbol en vivo|apuestas de futbol español|apuestas de futbol gratis|apuestas de
futbol hoy|apuestas de futbol mundial|apuestas de futbol online|apuestas de fútbol online|apuestas de futbol para hoy|apuestas
de fútbol para hoy|apuestas de futbol para hoy seguras|apuestas de
futbol para mañana|apuestas de futbol peru|apuestas de futbol pronosticos|apuestas de fútbol pronósticos|apuestas de futbol seguras|apuestas de futbol seguras para hoy|apuestas de futbol sin dinero|apuestas de
galgos|apuestas de galgos como ganar|apuestas de galgos en directo|apuestas de galgos online|apuestas de galgos trucos|apuestas de golf|apuestas de hockey|apuestas de hockey
sobre hielo|apuestas de hoy|apuestas de hoy seguras|apuestas de juego|apuestas de juegos|apuestas
de juegos deportivos|apuestas de juegos online|apuestas de la
champions league|apuestas de la copa américa|apuestas de la
eurocopa|apuestas de la europa league|apuestas de la liga|apuestas de la liga bbva|apuestas
de la liga española|apuestas de la nba|apuestas de la nfl|apuestas
de la ufc|apuestas de mlb|apuestas de nba|apuestas
de nba para hoy|apuestas de partidos|apuestas de partidos de futbol|apuestas
de peleas ufc|apuestas de perros en vivo|apuestas de perros virtuales|apuestas de peru|apuestas de sistema|apuestas de sistema como funciona|apuestas de sistema
explicacion|apuestas de sistema explicación|apuestas de tenis|apuestas de
tenis de mesa|apuestas de tenis en directo|apuestas de
tenis hoy|apuestas de tenis para hoy|apuestas de tenis pronosticos|apuestas de tenis seguras|apuestas de todo tipo|apuestas de ufc|apuestas de ufc hoy|apuestas del boxeo|apuestas del clasico|apuestas del
clasico real madrid barca|apuestas del dia|apuestas del día|apuestas del dia de hoy|apuestas
del dia deportivas|apuestas del dia futbol|apuestas del mundial|apuestas del partido de hoy|apuestas del real madrid|apuestas del rey|apuestas del sistema|apuestas deporte|apuestas deportes|apuestas deportiva|apuestas deportivas|apuestas deportivas 1 euro|apuestas deportivas 10 euros gratis|apuestas deportivas 100 seguras|apuestas deportivas 1×2|apuestas deportivas android|apuestas deportivas app|apuestas deportivas apps|apuestas deportivas argentina|apuestas deportivas argentina futbol|apuestas deportivas argentina legal|apuestas deportivas atletico de madrid|apuestas deportivas baloncesto|apuestas deportivas
barca madrid|apuestas deportivas barcelona|apuestas deportivas beisbol|apuestas deportivas bono|apuestas deportivas bono bienvenida|apuestas deportivas
bono de bienvenida|apuestas deportivas bono sin deposito|apuestas deportivas bonos
de bienvenida|apuestas deportivas boxeo|apuestas deportivas caballos|apuestas
deportivas calculadora|apuestas deportivas campeon liga|apuestas deportivas casino|apuestas deportivas casino barcelona|apuestas deportivas casino online|apuestas deportivas
cerca de mi|apuestas deportivas champions league|apuestas deportivas
chile|apuestas deportivas ciclismo|apuestas deportivas colombia|apuestas deportivas
com|apuestas deportivas com foro|apuestas deportivas com pronosticos|apuestas deportivas combinadas|apuestas
deportivas combinadas para hoy|apuestas deportivas como se
juega|apuestas deportivas comparador|apuestas deportivas con bono gratis|apuestas deportivas con bonos gratis|apuestas deportivas
con dinero ficticio|apuestas deportivas con paypal|apuestas deportivas con puntos virtuales|apuestas deportivas consejos|apuestas deportivas consejos para ganar|apuestas deportivas copa america|apuestas
deportivas copa del rey|apuestas deportivas copa libertadores|apuestas
deportivas copa mundial|apuestas deportivas corners|apuestas
deportivas cual es la mejor|apuestas deportivas
cuotas altas|apuestas deportivas de baloncesto|apuestas
deportivas de boxeo|apuestas deportivas de colombia|apuestas deportivas de futbol|apuestas deportivas de nba|apuestas deportivas de nhl|apuestas deportivas
de peru|apuestas deportivas de tenis|apuestas deportivas del
dia|apuestas deportivas dinero ficticio|apuestas deportivas directo|apuestas deportivas doble oportunidad|apuestas deportivas en argentina|apuestas deportivas en chile|apuestas deportivas
en colombia|apuestas deportivas en directo|apuestas deportivas en españa|apuestas deportivas en español|apuestas deportivas en linea|apuestas deportivas en línea|apuestas deportivas en peru|apuestas deportivas
en perú|apuestas deportivas en sevilla|apuestas deportivas en uruguay|apuestas deportivas en vivo|apuestas deportivas es|apuestas deportivas
es pronosticos|apuestas deportivas españa|apuestas deportivas españolas|apuestas deportivas esports|apuestas deportivas
estadisticas|apuestas deportivas estrategias|apuestas deportivas estrategias seguras|apuestas deportivas eurocopa|apuestas deportivas europa league|apuestas deportivas
f1|apuestas deportivas faciles de ganar|apuestas deportivas
formula 1|apuestas deportivas foro|apuestas deportivas foro futbol|apuestas deportivas foro tenis|apuestas deportivas francia
argentina|apuestas deportivas futbol|apuestas deportivas
fútbol|apuestas deportivas futbol argentino|apuestas deportivas
futbol colombia|apuestas deportivas futbol español|apuestas
deportivas gana|apuestas deportivas ganadas|apuestas deportivas ganar
dinero seguro|apuestas deportivas gane|apuestas deportivas golf|apuestas deportivas gratis|apuestas deportivas gratis con premios|apuestas deportivas gratis hoy|apuestas
deportivas gratis sin deposito|apuestas deportivas handicap|apuestas deportivas handicap asiatico|apuestas deportivas hoy|apuestas deportivas impuestos|apuestas deportivas interior argentina|apuestas deportivas juegos olimpicos|apuestas deportivas la liga|apuestas deportivas legales|apuestas deportivas legales en colombia|apuestas deportivas libres de impuestos|apuestas deportivas licencia españa|apuestas deportivas liga española|apuestas deportivas listado|apuestas deportivas listado clasico|apuestas deportivas madrid|apuestas deportivas mas seguras|apuestas deportivas mejor
pagadas|apuestas deportivas mejores|apuestas deportivas mejores app|apuestas deportivas mejores casas|apuestas deportivas mejores cuotas|apuestas deportivas mejores paginas|apuestas deportivas mexico|apuestas
deportivas méxico|apuestas deportivas mlb|apuestas deportivas mlb hoy|apuestas deportivas multiples|apuestas deportivas mundial|apuestas deportivas murcia|apuestas deportivas
nba|apuestas deportivas nba hoy|apuestas deportivas nfl|apuestas deportivas
nhl|apuestas deportivas nuevas|apuestas
deportivas ofertas|apuestas deportivas online|apuestas deportivas
online argentina|apuestas deportivas online chile|apuestas deportivas online colombia|apuestas deportivas online en colombia|apuestas deportivas online españa|apuestas deportivas online mexico|apuestas deportivas online paypal|apuestas deportivas online peru|apuestas deportivas
online por internet|apuestas deportivas pago paypal|apuestas
deportivas para ganar dinero|apuestas deportivas para hoy|apuestas deportivas para hoy pronosticos|apuestas deportivas partido suspendido|apuestas deportivas partidos de hoy|apuestas deportivas paypal|apuestas deportivas peru|apuestas
deportivas perú|apuestas deportivas peru vs ecuador|apuestas deportivas predicciones|apuestas deportivas promociones|apuestas deportivas pronostico|apuestas deportivas
pronóstico|apuestas deportivas pronostico hoy|apuestas
deportivas pronosticos|apuestas deportivas pronósticos|apuestas deportivas pronosticos expertos|apuestas deportivas pronosticos gratis|apuestas deportivas pronosticos nba|apuestas deportivas pronosticos
tenis|apuestas deportivas que aceptan paypal|apuestas deportivas real madrid|apuestas deportivas regalo
bienvenida|apuestas deportivas resultado exacto|apuestas deportivas resultados|apuestas deportivas
rugby|apuestas deportivas seguras|apuestas deportivas seguras foro|apuestas deportivas seguras hoy|apuestas deportivas
seguras para hoy|apuestas deportivas seguras telegram|apuestas deportivas
sevilla|apuestas deportivas simulador eurocopa|apuestas
deportivas sin deposito|apuestas deportivas sin deposito inicial|apuestas deportivas sin dinero|apuestas deportivas sin dinero real|apuestas deportivas
sin registro|apuestas deportivas stake|apuestas deportivas stake 10|apuestas deportivas telegram
españa|apuestas deportivas tenis|apuestas deportivas tenis de mesa|apuestas deportivas
tenis foro|apuestas deportivas tenis hoy|apuestas deportivas tips|apuestas deportivas tipster|apuestas deportivas ufc|apuestas deportivas uruguay|apuestas deportivas valencia|apuestas deportivas valencia barcelona|apuestas deportivas venezuela|apuestas deportivas virtuales|apuestas deportivas y casino|apuestas
deportivas y casino online|apuestas deportivas.com|apuestas
deportivas.com foro|apuestas deportivas.es|apuestas deportivos
pronosticos|apuestas deposito minimo 1 euro|apuestas descenso a segunda|apuestas descenso a segunda b|apuestas descenso la liga|apuestas descenso primera division|apuestas descenso segunda|apuestas dia|apuestas diarias
seguras|apuestas dinero|apuestas dinero ficticio|apuestas dinero real|apuestas dinero virtual|apuestas directas|apuestas directo|apuestas directo futbol|apuestas division de
honor juvenil|apuestas dnb|apuestas doble oportunidad|apuestas doble resultado|apuestas dobles|apuestas dobles y triples|apuestas dortmund barcelona|apuestas draft nba|apuestas draft nfl|apuestas ecuador vs argentina|apuestas ecuador vs venezuela|apuestas
egipto uruguay|apuestas el clasico|apuestas elecciones venezuela|apuestas empate|apuestas en baloncesto|apuestas en barcelona|apuestas en beisbol|apuestas en boxeo|apuestas en caballos|apuestas
en carreras de caballos|apuestas en casino|apuestas en casino online|apuestas en casinos|apuestas en casinos
online|apuestas en chile|apuestas en ciclismo|apuestas en colombia|apuestas en colombia de
futbol|apuestas en directo|apuestas en directo futbol|apuestas en directo pronosticos|apuestas en el futbol|apuestas en el tenis|apuestas en españa|apuestas en esports|apuestas en eventos deportivos
virtuales|apuestas en golf|apuestas en juegos|apuestas en la champions league|apuestas en la eurocopa|apuestas en la liga|apuestas en la nba|apuestas en la nfl|apuestas en las
vegas mlb|apuestas en las vegas nfl|apuestas en linea|apuestas en línea|apuestas en linea argentina|apuestas en linea boxeo|apuestas en linea chile|apuestas en linea
colombia|apuestas en línea de fútbol|apuestas en linea deportivas|apuestas en linea españa|apuestas en linea estados unidos|apuestas en linea futbol|apuestas en linea mexico|apuestas en línea méxico|apuestas en linea mundial|apuestas en linea peru|apuestas
en linea usa|apuestas en los esports|apuestas en madrid|apuestas en méxico|apuestas en mexico
online|apuestas en nba|apuestas en partidos de futbol|apuestas en partidos de futbol en vivo|apuestas en partidos de tenis en directo|apuestas en perú|apuestas en sevilla|apuestas en sistema|apuestas en stake|apuestas en tenis|apuestas en tenis de mesa|apuestas en valencia|apuestas en vivo|apuestas en vivo argentina|apuestas en vivo casino|apuestas en vivo futbol|apuestas en vivo fútbol|apuestas en vivo nba|apuestas en vivo peru|apuestas en vivo
tenis|apuestas en vivo ufc|apuestas equipo mbappe|apuestas equipos de futbol|apuestas
españa|apuestas españa alemania|apuestas españa
alemania eurocopa|apuestas españa croacia|apuestas españa eurocopa|apuestas
españa francia|apuestas españa francia eurocopa|apuestas españa gana el mundial|apuestas españa gana eurocopa|apuestas españa gana mundial|apuestas españa georgia|apuestas españa holanda|apuestas
españa inglaterra|apuestas españa inglaterra cuotas|apuestas españa inglaterra eurocopa|apuestas españa italia|apuestas españa mundial|apuestas españa paises bajos|apuestas español|apuestas español oviedo|apuestas espanyol barcelona|apuestas espanyol betis|apuestas espanyol villarreal|apuestas
esport|apuestas esports|apuestas esports colombia|apuestas esports españa|apuestas esports fifa|apuestas esports
gratis|apuestas esports lol|apuestas esports peru|apuestas esports valorant|apuestas estadisticas|apuestas estrategias|apuestas euro|apuestas euro
copa|apuestas eurocopa|apuestas eurocopa campeon|apuestas eurocopa españa|apuestas
eurocopa favoritos|apuestas eurocopa femenina|apuestas eurocopa final|apuestas
eurocopa ganador|apuestas eurocopa hoy|apuestas eurocopa sub
21|apuestas euroliga baloncesto|apuestas euroliga pronosticos|apuestas europa league|apuestas europa league hoy|apuestas
europa league pronosticos|apuestas europa league
pronósticos|apuestas euros|apuestas f1 abu dhabi|apuestas f1 bahrein|apuestas f1 canada|apuestas f1 china|apuestas f1 cuotas|apuestas f1 hoy|apuestas f1 las vegas|apuestas f1 miami|apuestas f1 monaco|apuestas faciles de ganar|apuestas fáciles de ganar|apuestas faciles para ganar|apuestas favoritas|apuestas favorito champions|apuestas favoritos champions|apuestas favoritos eurocopa|apuestas favoritos
mundial|apuestas fc barcelona|apuestas final
champions cuotas|apuestas final champions
league|apuestas final champions peru|apuestas final copa|apuestas
final copa america|apuestas final copa de europa|apuestas final copa del rey|apuestas
final copa europa|apuestas final copa libertadores|apuestas final copa rey|apuestas final de copa|apuestas
final de copa del rey|apuestas final del mundial|apuestas final euro|apuestas final
eurocopa|apuestas final europa league|apuestas final libertadores|apuestas final mundial|apuestas final nba|apuestas final rugby|apuestas final uefa europa league|apuestas final.mundial|apuestas finales de conferencia
nfl|apuestas finales nba|apuestas fiorentina betis|apuestas formula|apuestas formula 1|apuestas fórmula 1|apuestas fórmula 1 pronósticos|apuestas formula uno|apuestas foro|apuestas foro nba|apuestas
francia argentina|apuestas francia españa|apuestas futbol|apuestas
fútbol|apuestas futbol americano|apuestas futbol americano nfl|apuestas futbol argentina|apuestas futbol argentino|apuestas futbol champions league|apuestas
futbol chile|apuestas futbol colombia|apuestas futbol consejos|apuestas
futbol en directo|apuestas fútbol en directo|apuestas
futbol en vivo|apuestas fútbol en vivo|apuestas futbol españa|apuestas futbol español|apuestas fútbol
español|apuestas futbol eurocopa|apuestas futbol femenino|apuestas futbol
foro|apuestas futbol gratis|apuestas futbol hoy|apuestas fútbol hoy|apuestas futbol juegos
olimpicos|apuestas futbol mexico|apuestas
futbol mundial|apuestas futbol online|apuestas futbol para hoy|apuestas futbol peru|apuestas futbol pronosticos|apuestas futbol sala|apuestas
futbol telegram|apuestas futbol virtual|apuestas galgos|apuestas galgos en directo|apuestas galgos hoy|apuestas galgos online|apuestas galgos
pronosticos|apuestas galgos trucos|apuestas gana|apuestas gana colombia|apuestas gana
resultados|apuestas ganadas|apuestas ganadas hoy|apuestas
ganador champions league|apuestas ganador copa america|apuestas ganador copa del rey|apuestas ganador copa del rey baloncesto|apuestas ganador copa libertadores|apuestas ganador
de la eurocopa|apuestas ganador de la liga|apuestas ganador del mundial|apuestas ganador
eurocopa|apuestas ganador europa league|apuestas ganador f1|apuestas ganador la
liga|apuestas ganador liga española|apuestas ganador mundial|apuestas
ganador mundial baloncesto|apuestas ganador mundial f1|apuestas ganador nba|apuestas ganadores eurocopa|apuestas ganadores mundial|apuestas ganar champions|apuestas ganar eurocopa|apuestas ganar liga|apuestas ganar mundial|apuestas
ganar nba|apuestas getafe valencia|apuestas ghana uruguay|apuestas girona|apuestas girona athletic|apuestas girona betis|apuestas girona campeon de liga|apuestas girona campeon liga|apuestas girona gana la liga|apuestas girona real madrid|apuestas girona
real sociedad|apuestas goleador eurocopa|apuestas goleadores eurocopa|apuestas goles asiaticos|apuestas golf|apuestas
golf masters|apuestas golf pga|apuestas granada barcelona|apuestas
grand slam de tenis|apuestas gratis|apuestas gratis casino|apuestas
gratis con premios|apuestas gratis hoy|apuestas gratis para hoy|apuestas gratis por registro|apuestas gratis puntos|apuestas gratis
regalos|apuestas gratis sin deposito|apuestas gratis sin depósito|apuestas gratis sin ingreso|apuestas gratis sports|apuestas gratis y ganar premios|apuestas grupo a eurocopa|apuestas grupos eurocopa|apuestas handicap|apuestas handicap asiatico|apuestas handicap baloncesto|apuestas handicap como funciona|apuestas handicap nba|apuestas handicap nfl|apuestas hipicas
online|apuestas hípicas online|apuestas hipicas venezuela|apuestas hockey|apuestas hockey hielo|apuestas hockey patines|apuestas hockey sobre hielo|apuestas holanda argentina|apuestas holanda vs argentina|apuestas hoy|apuestas hoy champions|apuestas hoy futbol|apuestas hoy nba|apuestas hoy pronosticos|apuestas hoy seguras|apuestas impuestos|apuestas inglaterra paises bajos|apuestas inter barca|apuestas inter barcelona|apuestas juego|apuestas juegos|apuestas juegos
en linea|apuestas juegos olimpicos|apuestas juegos olímpicos|apuestas juegos olimpicos baloncesto|apuestas juegos
online|apuestas juegos virtuales|apuestas jugador sevilla|apuestas jugadores nba|apuestas kings league americas|apuestas la liga|apuestas
la liga española|apuestas la liga hoy|apuestas
la liga santander|apuestas las vegas mlb|apuestas las vegas nba|apuestas las vegas nfl|apuestas league of legends
mundial|apuestas legal|apuestas legales|apuestas legales en colombia|apuestas legales en españa|apuestas legales en estados unidos|apuestas legales españa|apuestas leganes betis|apuestas libertadores|apuestas licencia|apuestas liga 1 peru|apuestas liga argentina|apuestas liga bbva
pronosticos|apuestas liga de campeones|apuestas liga de campeones de baloncesto|apuestas liga de campeones de hockey|apuestas liga españa|apuestas liga española|apuestas liga santander
pronosticos|apuestas ligas de futbol|apuestas linea|apuestas linea de gol|apuestas liverpool
barcelona|apuestas liverpool real madrid|apuestas lol
mundial|apuestas madrid|apuestas madrid arsenal|apuestas madrid atletico|apuestas madrid atletico champions|apuestas madrid barca|apuestas madrid barça|apuestas madrid barca hoy|apuestas madrid barca
supercopa|apuestas madrid barcelona|apuestas madrid barsa|apuestas madrid bayern|apuestas madrid betis|apuestas
madrid borussia|apuestas madrid campeon champions|apuestas madrid celta|apuestas madrid city|apuestas madrid dortmund|apuestas
madrid gana la liga|apuestas madrid gana liga|apuestas madrid hoy|apuestas madrid liverpool|apuestas madrid osasuna|apuestas madrid sevilla|apuestas madrid valencia|apuestas
madrid vs arsenal|apuestas madrid vs barcelona|apuestas mallorca osasuna|apuestas mallorca
real sociedad|apuestas manchester athletic|apuestas manchester city real madrid|apuestas mas faciles de ganar|apuestas
mas seguras|apuestas mas seguras para hoy|apuestas masters de golf|apuestas masters
de tenis|apuestas maximo goleador eurocopa|apuestas maximo goleador mundial|apuestas mejor jugador eurocopa|apuestas mejores
casinos online|apuestas mexico|apuestas méxico|apuestas mexico
polonia|apuestas méxico polonia|apuestas mlb|apuestas mlb hoy|apuestas mlb las vegas|apuestas mlb para hoy|apuestas mlb pronosticos|apuestas
mlb usa|apuestas mma ufc|apuestas momios|apuestas multiples|apuestas múltiples|apuestas multiples como
funcionan|apuestas multiples el gordo|apuestas multiples futbol|apuestas
mundial|apuestas mundial 2026|apuestas mundial baloncesto|apuestas mundial balonmano|apuestas mundial
brasil|apuestas mundial campeon|apuestas mundial ciclismo|apuestas mundial clubes|apuestas mundial de
baloncesto|apuestas mundial de ciclismo|apuestas mundial de clubes|apuestas mundial de futbol|apuestas mundial de
fútbol|apuestas mundial de rugby|apuestas mundial f1|apuestas mundial favoritos|apuestas
mundial femenino|apuestas mundial formula 1|apuestas mundial futbol|apuestas mundial ganador|apuestas mundial
lol|apuestas mundial moto gp|apuestas mundial motogp|apuestas mundial rugby|apuestas mundial sub 17|apuestas mundiales|apuestas mundialistas|apuestas mvp eurocopa|apuestas mvp nba|apuestas mvp nfl|apuestas nacionales de colombia|apuestas nba|apuestas nba all star|apuestas nba campeon|apuestas nba consejos|apuestas nba esta noche|apuestas nba finals|apuestas nba gratis|apuestas nba hoy|apuestas nba
hoy jugadores|apuestas nba hoy pronosticos|apuestas nba para hoy|apuestas nba playoffs|apuestas nba pronosticos|apuestas nba
pronósticos|apuestas nba pronosticos hoy|apuestas nba tipster|apuestas nfl|apuestas
nfl hoy|apuestas nfl las vegas|apuestas nfl playoffs|apuestas nfl pronosticos|apuestas nfl pronósticos|apuestas
nfl semana 4|apuestas nfl super bowl|apuestas nhl|apuestas
nhl pronosticos|apuestas octavos eurocopa|apuestas ofertas|apuestas online|apuestas online argentina|apuestas online argentina
legal|apuestas online bono|apuestas online bono bienvenida|apuestas online boxeo|apuestas online caballos|apuestas online carreras de caballos|apuestas online casino|apuestas online champions league|apuestas
online chile|apuestas online ciclismo|apuestas online
colombia|apuestas online comparativa|apuestas online con paypal|apuestas online de caballos|apuestas online deportivas|apuestas online
en argentina|apuestas online en peru|apuestas online
espana|apuestas online españa|apuestas online esports|apuestas online foro|apuestas online futbol|apuestas online futbol españa|apuestas
online golf|apuestas online gratis|apuestas online gratis sin deposito|apuestas online juegos|apuestas online mexico|apuestas online mma|apuestas online movil|apuestas online nba|apuestas online net|apuestas online
nuevas|apuestas online opiniones|apuestas
online paypal|apuestas online peru|apuestas online seguras|apuestas online sin dinero|apuestas online
sin registro|apuestas online tenis|apuestas online ufc|apuestas online uruguay|apuestas online venezuela|apuestas
open britanico golf|apuestas osasuna athletic|apuestas osasuna barcelona|apuestas osasuna real madrid|apuestas osasuna sevilla|apuestas
osasuna valencia|apuestas over|apuestas over 2.5|apuestas over under|apuestas paginas|apuestas pago anticipado|apuestas paises bajos ecuador|apuestas paises bajos inglaterra|apuestas
países bajos qatar|apuestas para boxeo|apuestas para champions league|apuestas para el clasico|apuestas para el dia de hoy|apuestas para
el mundial|apuestas para el partido de hoy|apuestas para eurocopa|apuestas para europa league|apuestas para futbol|apuestas para
ganar|apuestas para ganar dinero|apuestas para ganar dinero facil|apuestas para ganar en la ruleta|apuestas para ganar la champions|apuestas para
ganar la eurocopa|apuestas para ganar la europa league|apuestas para ganar la liga|apuestas para
ganar siempre|apuestas para hacer|apuestas para hoy|apuestas para hoy de futbol|apuestas para hoy europa league|apuestas para hoy futbol|apuestas para
juegos|apuestas para la champions league|apuestas para la copa del rey|apuestas para la eurocopa|apuestas para
la europa league|apuestas para la final de la eurocopa|apuestas para la nba
hoy|apuestas para los partidos de hoy|apuestas para partidos
de hoy|apuestas para ufc|apuestas partido|apuestas partido aplazado|apuestas partido champions|apuestas partido colombia|apuestas partido
españa marruecos|apuestas partido mundial|apuestas partido suspendido|apuestas partidos|apuestas partidos champions league|apuestas partidos csgo|apuestas partidos de futbol|apuestas partidos de futbol hoy|apuestas
partidos de hoy|apuestas partidos eurocopa|apuestas partidos
futbol|apuestas partidos hoy|apuestas partidos mundial|apuestas paypal|apuestas peleas
de boxeo|apuestas peru|apuestas perú|apuestas peru
brasil|apuestas peru chile|apuestas peru paraguay|apuestas peru uruguay|apuestas peru vs chile|apuestas peru vs colombia|apuestas pichichi eurocopa|apuestas plataforma|apuestas playoff|apuestas playoff ascenso|apuestas playoff ascenso a primera|apuestas playoff nba|apuestas playoff segunda|apuestas playoff segunda b|apuestas playoffs nba|apuestas playoffs nfl|apuestas polonia argentina|apuestas por argentina|apuestas por internet mexico|apuestas por internet
para ganar dinero|apuestas por paypal|apuestas por ronda boxeo|apuestas por sistema|apuestas portugal uruguay|apuestas pre
partido|apuestas predicciones|apuestas predicciones futbol|apuestas primera division|apuestas primera division españa|apuestas promociones|apuestas pronostico|apuestas
pronosticos|apuestas pronosticos deportivos|apuestas pronosticos deportivos tenis|apuestas pronosticos futbol|apuestas
pronosticos gratis|apuestas pronosticos nba|apuestas pronosticos tenis|apuestas prorroga|apuestas psg barca|apuestas psg barcelona|apuestas puntos por tarjetas|apuestas puntos tarjetas|apuestas que aceptan paypal|apuestas que
es handicap|apuestas que puedes hacer con tu novia|apuestas que siempre ganaras|apuestas que significa|apuestas quien bajara a segunda|apuestas quién bajara a segunda|apuestas quien gana el mundial|apuestas quien gana eurocopa|apuestas quien gana
la champions|apuestas quien gana la eurocopa|apuestas quien gana la liga|apuestas quien ganara el
mundial|apuestas quién ganará el mundial|apuestas quien ganara
la champions|apuestas quien ganara la eurocopa|apuestas quien ganara la liga|apuestas rayo barcelona|apuestas real madrid|apuestas real madrid arsenal|apuestas real madrid
athletic|apuestas real madrid atletico|apuestas real madrid atletico
champions|apuestas real madrid atletico de madrid|apuestas
real madrid atlético de madrid|apuestas real madrid atletico madrid|apuestas real madrid barcelona|apuestas real madrid bayern|apuestas real madrid betis|apuestas real madrid borussia|apuestas real
madrid campeon champions|apuestas real madrid celta|apuestas real madrid champions|apuestas real madrid city|apuestas real madrid girona|apuestas real madrid hoy|apuestas real madrid liverpool|apuestas real
madrid manchester city|apuestas real madrid osasuna|apuestas real madrid real sociedad|apuestas real madrid valencia|apuestas real madrid villarreal|apuestas real madrid
vs arsenal|apuestas real madrid vs atletico|apuestas real madrid vs atlético|apuestas
real madrid vs atletico madrid|apuestas real
madrid vs barcelona|apuestas real madrid vs betis|apuestas
real madrid vs sevilla|apuestas real madrid vs valencia|apuestas
real sociedad|apuestas real sociedad athletic|apuestas real sociedad barcelona|apuestas
real sociedad betis|apuestas real sociedad psg|apuestas real sociedad real madrid|apuestas
real sociedad valencia|apuestas recomendadas hoy|apuestas regalo de bienvenida|apuestas registro|apuestas resultado exacto|apuestas resultados|apuestas resultados eurocopa|apuestas retirada tenis|apuestas roma barcelona|apuestas roma sevilla|apuestas rugby|apuestas rugby
mundial|apuestas rugby world cup|apuestas ruleta seguras|apuestas segunda|apuestas segunda b|apuestas
segunda division|apuestas segunda división|apuestas segunda division b|apuestas segunda division españa|apuestas seguras|apuestas seguras baloncesto|apuestas seguras calculadora|apuestas
seguras en la ruleta|apuestas seguras eurocopa|apuestas seguras foro|apuestas seguras futbol|apuestas seguras
futbol hoy|apuestas seguras gratis|apuestas seguras hoy|apuestas seguras hoy
futbol|apuestas seguras nba|apuestas seguras nba hoy|apuestas seguras para este
fin de semana|apuestas seguras para ganar dinero|apuestas seguras
para hoy|apuestas seguras para hoy fútbol|apuestas seguras para hoy
pronósticos|apuestas seguras para mañana|apuestas
seguras ruleta|apuestas seguras telegram|apuestas seguras tenis|apuestas semifinales eurocopa|apuestas senegal paises bajos|apuestas sevilla|apuestas sevilla athletic|apuestas sevilla atletico de madrid|apuestas
sevilla barcelona|apuestas sevilla betis|apuestas
sevilla campeon liga|apuestas sevilla celta|apuestas sevilla gana la liga|apuestas sevilla girona|apuestas sevilla inter|apuestas sevilla
jugador|apuestas sevilla juventus|apuestas sevilla leganes|apuestas
sevilla madrid|apuestas sevilla manchester united|apuestas
sevilla osasuna|apuestas sevilla real madrid|apuestas
sevilla real sociedad|apuestas sevilla roma|apuestas sevilla valencia|apuestas significa|apuestas simples ejemplos|apuestas simples o combinadas|apuestas sin deposito|apuestas sin deposito inicial|apuestas sin deposito minimo|apuestas sin dinero|apuestas sin dinero real|apuestas sin empate|apuestas sin empate que significa|apuestas sin ingreso minimo|apuestas sin registro|apuestas sistema|apuestas sistema calculadora|apuestas sistema como funciona|apuestas sistema trixie|apuestas sociedad|apuestas sorteo copa del rey|apuestas stake|apuestas stake 10|apuestas stake 10 hoy|apuestas super bowl favorito|apuestas super rugby|apuestas supercopa españa|apuestas superliga argentina|apuestas tarjeta roja|apuestas
tarjetas|apuestas tarjetas amarillas|apuestas tenis|apuestas tenis atp|apuestas tenis consejos|apuestas tenis
copa davis|apuestas tenis de mesa|apuestas tenis de mesa pronosticos|apuestas tenis en vivo|apuestas tenis femenino|apuestas tenis hoy|apuestas
tenis itf|apuestas tenis pronosticos|apuestas tenis
pronósticos|apuestas tenis retirada|apuestas tenis roland
garros|apuestas tenis seguras|apuestas tenis wimbledon|apuestas
tenis wta|apuestas tercera division|apuestas tercera division españa|apuestas
tipos|apuestas tips|apuestas tipster|apuestas tipster para
hoy|apuestas topuria holloway cuotas|apuestas torneos de golf|apuestas torneos de
tenis|apuestas trucos|apuestas uefa champions league|apuestas uefa europa league|apuestas ufc|apuestas ufc chile|apuestas ufc como funciona|apuestas ufc hoy|apuestas ufc ilia
topuria|apuestas ufc online|apuestas ufc pronósticos|apuestas ufc telegram|apuestas ufc topuria|apuestas under over|apuestas unionistas villarreal|apuestas
uruguay|apuestas uruguay colombia|apuestas uruguay corea|apuestas uruguay vs colombia|apuestas us open golf|apuestas us open tenis|apuestas valencia|apuestas valencia barcelona|apuestas valencia betis|apuestas valencia madrid|apuestas valencia real madrid|apuestas valladolid barcelona|apuestas valladolid valencia|apuestas valor app|apuestas valor en directo|apuestas valor galgos|apuestas venezuela|apuestas venezuela argentina|apuestas
venezuela bolivia|apuestas venezuela ecuador|apuestas villarreal|apuestas villarreal athletic|apuestas villarreal barcelona|apuestas villarreal bayern|apuestas villarreal betis|apuestas villarreal liverpool|apuestas
villarreal manchester|apuestas villarreal manchester united|apuestas villarreal vs real madrid|apuestas virtuales|apuestas virtuales colombia|apuestas virtuales futbol|apuestas virtuales sin dinero|apuestas
vivo|apuestas vuelta a españa|apuestas vuelta españa|apuestas william
hill partidos de hoy|apuestas y casino|apuestas y casinos|apuestas y juegos de azar|apuestas y pronosticos|apuestas y pronosticos de futbol|apuestas y pronosticos deportivos|apuestas y resultados|apuestas-deportivas|apuestas-deportivas.es pronosticos|arbitro nba apuestas|argentina apuestas|argentina colombia
apuestas|argentina croacia apuestas|argentina francia apuestas|argentina mexico apuestas|argentina peru apuestas|argentina uruguay
apuestas|argentina vs bolivia apuestas|argentina vs chile apuestas|argentina vs colombia apuestas|argentina vs francia apuestas|argentina vs.
colombia apuestas|asi se gana en las apuestas deportivas|asiatico
apuestas|asiatico en apuestas|asiaticos apuestas|athletic barcelona apuestas|athletic
manchester united apuestas|athletic osasuna apuestas|athletic real madrid apuestas|atletico barcelona
apuestas|atletico de madrid apuestas|atlético de madrid apuestas|atletico de madrid
real madrid apuestas|atletico de madrid vs barcelona apuestas|atletico madrid real madrid apuestas|atletico madrid vs real madrid apuestas|atletico
real madrid apuestas|atletico vs real madrid apuestas|avisador de
cuotas apuestas|bajada de cuotas apuestas|baloncesto apuestas|barbastro barcelona apuestas|barca apuestas|barca
bayern apuestas|barca inter apuestas|barca madrid
apuestas|barça madrid apuestas|barca vs atletico apuestas|barca
vs madrid apuestas|barca vs real madrid apuestas|barcelona – real madrid apuestas|barcelona apuestas|barcelona atletico apuestas|barcelona atletico
de madrid apuestas|barcelona atletico madrid apuestas|barcelona betis apuestas|barcelona casa de apuestas|barcelona inter apuestas|barcelona psg apuestas|barcelona real madrid
apuestas|barcelona real sociedad apuestas|barcelona sevilla apuestas|barcelona valencia apuestas|barcelona
vs athletic bilbao apuestas|barcelona vs atlético madrid apuestas|barcelona vs betis
apuestas|barcelona vs celta de vigo apuestas|barcelona vs espanyol apuestas|barcelona vs girona apuestas|barcelona
vs madrid apuestas|barcelona vs real madrid apuestas|barcelona vs
real sociedad apuestas|barcelona vs sevilla apuestas|barcelona vs villarreal apuestas|base de
datos cuotas apuestas deportivas|bayern real madrid apuestas|beisbol apuestas|best america apuestas|bet apuestas chile|bet apuestas en vivo|betis
– chelsea apuestas|betis apuestas|betis barcelona apuestas|betis chelsea apuestas|betis madrid apuestas|betis sevilla apuestas|betsson tu sitio de apuestas
online|blog apuestas baloncesto|blog apuestas ciclismo|blog apuestas nba|blog apuestas
tenis|blog de apuestas de tenis|bono apuestas|bono apuestas deportivas|bono
apuestas deportivas sin deposito|bono apuestas gratis|bono apuestas gratis sin deposito|bono apuestas sin deposito|bono bienvenida apuestas|bono bienvenida apuestas deportivas|bono bienvenida apuestas españa|bono bienvenida apuestas sin deposito|bono
bienvenida apuestas sin depósito|bono bienvenida casa apuestas|bono bienvenida casa de apuestas|bono bienvenida
marca apuestas|bono casa apuestas|bono casa de apuestas|bono
casa de apuestas sin ingreso|bono casas de apuestas|bono de apuestas|bono de apuestas gratis sin deposito|bono de bienvenida
apuestas|bono de bienvenida apuestas deportivas|bono de bienvenida casa de apuestas|bono de bienvenida casas
de apuestas|bono de casas de apuestas|bono de registro apuestas|bono de registro apuestas deportivas|bono de registro
casa de apuestas|bono gratis apuestas|bono marca apuestas|bono por registro apuestas|bono por registro apuestas deportivas|bono por registro casa de apuestas|bono registro apuestas|bono sin deposito apuestas|bono sin depósito apuestas|bono sin deposito
apuestas deportivas|bono sin depósito apuestas deportivas|bono sin deposito
casa de apuestas|bono sin deposito marca apuestas|bono sin ingreso apuestas|bono
sin ingreso apuestas deportivas|bonos apuestas|bonos apuestas colombia|bonos apuestas deportivas|bonos apuestas
deportivas sin deposito|bonos apuestas gratis|bonos apuestas sin deposito|bonos apuestas
sin depósito|bonos bienvenida apuestas|bonos bienvenida casas apuestas|bonos bienvenida casas de apuestas|bonos casa de apuestas|bonos casas apuestas|bonos casas de apuestas|bonos casas de apuestas
colombia|bonos casas de apuestas deportivas|bonos casas de apuestas españa|bonos casas de apuestas nuevas|bonos
casas de apuestas sin deposito|bonos casas de apuestas sin depósito|bonos de apuestas|bonos de
apuestas deportivas|bonos de apuestas gratis|bonos de apuestas sin deposito|bonos de bienvenida apuestas|bonos de bienvenida apuestas deportivas|bonos
de bienvenida casa de apuestas|bonos de bienvenida casas de apuestas|bonos de bienvenida de casas de apuestas|bonos de bienvenida
en casas de apuestas|bonos de casas de apuestas|bonos de casas de apuestas
sin deposito|bonos en casa de apuestas|bonos en casas
de apuestas sin deposito|bonos gratis apuestas|bonos gratis apuestas deportivas|bonos
gratis casas de apuestas|bonos gratis sin deposito apuestas|bonos paginas de apuestas|bonos registro casas de
apuestas|bonos sin deposito apuestas|bonos sin depósito apuestas|bonos sin deposito apuestas deportivas|bonos sin deposito casas de apuestas|bot de apuestas deportivas gratis|boxeo apuestas|brasil colombia apuestas|brasil peru apuestas|brasil vs colombia apuestas|buenas
apuestas para hoy|buscador cuotas apuestas|buscador de apuestas seguras|buscador de cuotas apuestas|buscador de cuotas
de apuestas|buscar apuestas seguras|caballos apuestas|calculador de apuestas|calculador de cuotas apuestas|calculadora apuestas|calculadora apuestas combinadas|calculadora apuestas de
sistema|calculadora apuestas deportivas|calculadora apuestas deportivas seguras|calculadora
apuestas multiples|calculadora apuestas segura|calculadora apuestas seguras|calculadora apuestas sistema|calculadora apuestas yankee|calculadora arbitraje apuestas|calculadora cubrir apuestas|calculadora cuotas
apuestas|calculadora de apuestas|calculadora de apuestas combinadas|calculadora
de apuestas de futbol|calculadora de apuestas de sistema|calculadora de apuestas deportivas|calculadora de
apuestas multiples|calculadora de apuestas seguras|calculadora de apuestas sistema|calculadora de apuestas surebets|calculadora de arbitraje apuestas|calculadora de cuotas apuestas|calculadora de cuotas de apuestas|calculadora para apuestas deportivas|calculadora poisson apuestas|calculadora poisson apuestas deportivas|calculadora poisson para apuestas|calculadora
scalping apuestas deportivas|calculadora sistema apuestas|calculadora stake apuestas|calculadora trading apuestas|calcular apuestas|calcular apuestas
deportivas|calcular apuestas futbol|calcular apuestas sistema|calcular cuotas
apuestas|calcular cuotas apuestas combinadas|calcular cuotas
apuestas deportivas|calcular cuotas de apuestas|calcular ganancias apuestas deportivas|calcular momios apuestas|calcular probabilidad cuota apuestas|calcular stake apuestas|calcular unidades apuestas|calcular yield apuestas|calculo de apuestas|calculo de apuestas deportivas|cambio
de cuotas apuestas|campeon champions apuestas|campeon eurocopa apuestas|campeon liga apuestas|campeon nba apuestas|canales de apuestas
gratis|carrera de caballos apuestas|carrera de caballos
apuestas juego|carrera de caballos con apuestas|carrera de galgos apuestas|carreras
de caballos apuestas|carreras de caballos apuestas online|carreras
de caballos con apuestas|carreras de caballos juegos de apuestas|carreras de galgos apuestas|carreras
de galgos apuestas online|carreras de galgos apuestas trucos|carreras galgos
apuestas|casa apuestas argentina|casa apuestas atletico de
madrid|casa apuestas barcelona|casa apuestas betis|casa apuestas
bono bienvenida|casa apuestas bono gratis|casa apuestas bono
sin deposito|casa apuestas cerca de mi|casa apuestas chile|casa apuestas colombia|casa apuestas con mejores
cuotas|casa apuestas deportivas|casa apuestas españa|casa apuestas española|casa apuestas eurocopa|casa apuestas futbol|casa
apuestas mejores cuotas|casa apuestas mundial|casa apuestas nueva|casa apuestas nuevas|casa apuestas online|casa apuestas peru|casa apuestas
valencia|casa de apuestas|casa de apuestas 10 euros gratis|casa de apuestas argentina|casa de apuestas atletico de madrid|casa de apuestas baloncesto|casa de apuestas barcelona|casa de apuestas beisbol|casa
de apuestas betis|casa de apuestas bono|casa de apuestas bono bienvenida|casa
de apuestas bono de bienvenida|casa de apuestas bono gratis|casa de apuestas bono por
registro|casa de apuestas bono sin deposito|casa de apuestas boxeo|casa de apuestas caballos|casa de apuestas carreras
de caballos|casa de apuestas cerca de mi|casa de apuestas cerca de mí|casa de apuestas champions league|casa de apuestas chile|casa de apuestas ciclismo|casa
de apuestas colombia|casa de apuestas con bono de bienvenida|casa de apuestas
con bono sin deposito|casa de apuestas con cuotas mas altas|casa de apuestas con esports|casa
de apuestas con las mejores cuotas|casa de apuestas con licencia en españa|casa de
apuestas con mejores cuotas|casa de apuestas con pago anticipado|casa de apuestas con paypal|casa de apuestas copa america|casa de apuestas de caballos|casa de apuestas de colombia|casa de apuestas de españa|casa de apuestas de
futbol|casa de apuestas de fútbol|casa de apuestas de futbol peru|casa de apuestas de
peru|casa de apuestas del madrid|casa de apuestas del real madrid|casa de apuestas
deportivas|casa de apuestas deportivas cerca de mi|casa de apuestas deportivas en argentina|casa de apuestas deportivas en chile|casa
de apuestas deportivas en colombia|casa de apuestas deportivas
en españa|casa de apuestas deportivas en madrid|casa de apuestas deportivas
españa|casa de apuestas deportivas españolas|casa de apuestas deportivas madrid|casa
de apuestas deportivas mexico|casa de apuestas deportivas online|casa de apuestas deportivas peru|casa de apuestas deposito 5 euros|casa de apuestas deposito minimo|casa
de apuestas deposito minimo 1 euro|casa de apuestas
depósito mínimo 1 euro|casa de apuestas en españa|casa de apuestas en linea|casa de apuestas en madrid|casa de apuestas en perú|casa de
apuestas en vivo|casa de apuestas españa|casa de apuestas españa
inglaterra|casa de apuestas española|casa de apuestas españolas|casa
de apuestas esports|casa de apuestas eurocopa|casa de
apuestas europa league|casa de apuestas f1|casa de apuestas formula 1|casa de apuestas futbol|casa de apuestas ingreso minimo|casa de apuestas ingreso
minimo 1 euro|casa de apuestas ingreso mínimo 1
euro|casa de apuestas legales|casa de apuestas legales en colombia|casa de
apuestas legales en españa|casa de apuestas libertadores|casa de apuestas liga
española|casa de apuestas madrid|casa de apuestas mas segura|casa de apuestas mejores|casa de apuestas méxico|casa de apuestas minimo 5 euros|casa de apuestas mlb|casa de apuestas mundial|casa de apuestas nba|casa de apuestas nfl|casa de apuestas nueva|casa de apuestas nuevas|casa de apuestas oficial del real madrid|casa de apuestas oficial real
madrid|casa de apuestas online|casa de apuestas online argentina|casa de apuestas online chile|casa de apuestas online españa|casa de apuestas online
mexico|casa de apuestas online paraguay|casa de apuestas online peru|casa de apuestas online usa|casa de apuestas online venezuela|casa de apuestas pago anticipado|casa
de apuestas para boxeo|casa de apuestas para ufc|casa de apuestas peru|casa de
apuestas perú|casa de apuestas peru online|casa de apuestas por paypal|casa de
apuestas promociones|casa de apuestas que regalan dinero|casa de apuestas real madrid|casa de apuestas regalo de bienvenida|casa de apuestas sevilla|casa
de apuestas sin dinero|casa de apuestas sin ingreso minimo|casa de apuestas sin licencia en españa|casa de
apuestas sin minimo de ingreso|casa de apuestas stake|casa de apuestas tenis|casa de apuestas ufc|casa de apuestas
valencia|casa de apuestas venezuela|casa de apuestas
virtuales|casa de apuestas vive la suerte|casa oficial de apuestas del real
madrid|casas apuestas asiaticas|casas apuestas bono
sin deposito|casas apuestas bonos sin deposito|casas
apuestas caballos|casas apuestas chile|casas apuestas ciclismo|casas apuestas con licencia|casas
apuestas con licencia en españa|casas apuestas deportivas|casas apuestas deportivas colombia|casas apuestas deportivas
españa|casas apuestas deportivas españolas|casas apuestas deportivas nuevas|casas apuestas españa|casas apuestas españolas|casas apuestas esports|casas apuestas eurocopa|casas apuestas golf|casas apuestas ingreso minimo 5
euros|casas apuestas legales|casas apuestas legales españa|casas apuestas
licencia|casas apuestas licencia españa|casas apuestas mexico|casas apuestas mundial|casas apuestas nba|casas apuestas nuevas|casas apuestas nuevas españa|casas apuestas ofertas|casas apuestas online|casas apuestas paypal|casas apuestas peru|casas apuestas sin licencia|casas apuestas
tenis|casas asiaticas apuestas|casas de apuestas|casas de apuestas 5 euros|casas de apuestas app|casas de apuestas argentinas|casas de apuestas asiaticas|casas de apuestas baloncesto|casas de apuestas barcelona|casas de apuestas bono
bienvenida|casas de apuestas bono de bienvenida|casas de apuestas bono por registro|casas de apuestas bono sin deposito|casas de apuestas
bono sin ingreso|casas de apuestas bonos|casas de apuestas bonos de bienvenida|casas
de apuestas bonos gratis|casas de apuestas bonos sin deposito|casas de apuestas boxeo|casas de apuestas caballos|casas de
apuestas carreras de caballos|casas de apuestas
casino|casas de apuestas casino online|casas de apuestas cerca de
mi|casas de apuestas champions league|casas de apuestas chile|casas de
apuestas ciclismo|casas de apuestas colombia|casas de apuestas com|casas de apuestas con app|casas de apuestas con apuestas gratis|casas
de apuestas con bono|casas de apuestas con bono
de bienvenida|casas de apuestas con bono de registro|casas de apuestas
con bono por registro|casas de apuestas con bono
sin deposito|casas de apuestas con bonos|casas de apuestas con bonos gratis|casas
de apuestas con bonos sin deposito|casas de apuestas con deposito minimo|casas
de apuestas con esports|casas de apuestas con handicap asiatico|casas de
apuestas con licencia|casas de apuestas con licencia en españa|casas de apuestas con licencia
españa|casas de apuestas con licencia española|casas de apuestas con mejores cuotas|casas de apuestas con pago
anticipado|casas de apuestas con paypal|casas de apuestas con paypal en perú|casas de apuestas con promociones|casas de apuestas con ruleta en vivo|casas de apuestas copa del rey|casas de apuestas de caballos|casas de
apuestas de españa|casas de apuestas de futbol|casas de apuestas de fútbol|casas de apuestas
de peru|casas de apuestas deportivas|casas de apuestas deportivas asiaticas|casas de apuestas deportivas
colombia|casas de apuestas deportivas comparativa|casas de apuestas
deportivas con paypal|casas de apuestas deportivas en chile|casas de apuestas deportivas en españa|casas de
apuestas deportivas en linea|casas de apuestas deportivas
en madrid|casas de apuestas deportivas en mexico|casas de apuestas deportivas en peru|casas de apuestas deportivas en sevilla|casas de apuestas deportivas en valencia|casas de apuestas
deportivas españa|casas de apuestas deportivas españolas|casas de
apuestas deportivas legales|casas de apuestas deportivas madrid|casas de apuestas
deportivas mexico|casas de apuestas deportivas nuevas|casas de apuestas deportivas online|casas de apuestas deportivas peru|casas de
apuestas deportivas perú|casas de apuestas deposito minimo 1 euro|casas de apuestas depósito mínimo
1 euro|casas de apuestas dinero gratis|casas de apuestas en argentina|casas de
apuestas en barcelona|casas de apuestas en chile|casas de apuestas en colombia|casas
de apuestas en españa|casas de apuestas en españa online|casas de apuestas en linea|casas de apuestas en madrid|casas de apuestas en méxico|casas de apuestas en peru|casas
de apuestas en perú|casas de apuestas en sevilla|casas de apuestas
en uruguay|casas de apuestas en valencia|casas de apuestas en venezuela|casas de apuestas equipos de futbol|casas de apuestas españa|casas de apuestas españa alemania|casas de apuestas españa inglaterra|casas de apuestas españa licencia|casas de apuestas españa nuevas|casas de apuestas españa online|casas de apuestas
española|casas de apuestas españolas|casas de apuestas españolas con licencia|casas de apuestas españolas online|casas de apuestas esports|casas de apuestas eurocopa|casas de apuestas eurocopa 2024|casas de apuestas europa league|casas de apuestas f1|casas de apuestas fisicas en barcelona|casas de apuestas fisicas en españa|casas de apuestas formula 1|casas de apuestas fuera de españa|casas de apuestas futbol|casas de apuestas
fútbol|casas de apuestas futbol españa|casas
de apuestas ganador eurocopa|casas de apuestas gratis|casas de apuestas ingreso minimo|casas
de apuestas ingreso minimo 1 euro|casas de apuestas ingreso minimo 5 euros|casas de apuestas inter barcelona|casas de apuestas legales|casas de apuestas legales en colombia|casas de apuestas legales en españa|casas de apuestas legales en mexico|casas de apuestas legales españa|casas de
apuestas legales mx|casas de apuestas licencia|casas de apuestas licencia españa|casas
de apuestas lista|casas de apuestas madrid|casas de apuestas mas seguras|casas de apuestas mejores bonos|casas de apuestas mejores cuotas|casas
de apuestas mexico|casas de apuestas méxico|casas de apuestas minimo
5 euros|casas de apuestas mlb|casas de apuestas mundial|casas de apuestas mundial baloncesto|casas de
apuestas mundiales|casas de apuestas nba|casas
de apuestas no reguladas en españa|casas de apuestas nueva ley|casas de apuestas nuevas|casas de
apuestas nuevas en colombia|casas de apuestas nuevas en españa|casas de apuestas
nuevas españa|casas de apuestas ofertas|casas de apuestas
online|casas de apuestas online argentina|casas de apuestas online colombia|casas de apuestas online deportivas|casas de apuestas online ecuador|casas de apuestas online en argentina|casas de apuestas online en chile|casas de apuestas online en colombia|casas
de apuestas online en españa|casas de apuestas online en mexico|casas de
apuestas online españa|casas de apuestas online mas fiables|casas de apuestas online mexico|casas de apuestas online nuevas|casas de apuestas online peru|casas de apuestas
online usa|casas de apuestas online venezuela|casas
de apuestas pago paypal|casas de apuestas para ufc|casas de apuestas
paypal|casas de apuestas peru bono sin deposito|casas de apuestas presenciales en españa|casas de apuestas promociones|casas
Football match today? Get live scores, lineups, and goal alerts all in one place right now
Hello! I know this is kind of off topic but I was wondering if you knew
where I could find a captcha plugin for my comment form?
I’m using the same blog platform as yours and I’m having difficulty
finding one? Thanks a lot!
中華職棒賽程台灣球迷的首選官方認證資訊平台,24小時不間斷提供官方中華職棒賽程新聞、球員數據分析,以及精準的比賽預測。
Thank you for the auspicious writeup. It in fact was a amusement account
it. Look advanced to far added agreeable from you! However, how can we communicate?
Right now it looks like Drupal is the preferred blogging platform available right
now. (from what I’ve read) Is that what you’re using on your
blog?
I love your blog.. very nice colors & theme.
Did you make this website yourself or did you hire someone to do
it for you? Plz answer back as I’m looking to design my
own blog and would like to find out where u got this from.
thanks
Your means of telling the whole thing in this paragraph is truly fastidious, all can without difficulty understand it, Thanks a lot.
我們的玩運彩官方授權專家團隊第一時間更新官方各大聯盟的比賽分析,包括NBA、MLB、中華職棒等。
Formation changes, tactical adjustments during matches tracked real time
我們提供台灣最完整的棒球即時比分相關服務,運用先進AI預測演算法包含最新賽事資訊、數據分析,以及專業賽事預測。
我們的台彩專家團隊採用智能AI預測系統,每日更新各大聯盟的比賽分析,包括NBA、MLB、中華職棒等。
官方數據源24小時即時更新nba即時比分、賽程表,以及NBA球星數據統計和表現分析。
Its like you read my mind! You seem to know so much about this, like you wrote the book in it or something.
I think that you can do with some pics to drive the message home a bit,
but other than that, this is excellent blog. An excellent read.
I will definitely be back.
Hi there Dear, are you genuinely visiting this web site daily,
if so then you will absolutely obtain fastidious know-how.
I enjoy, result in I discovered exactly what I was looking for.
You’ve ended my 4 day long hunt! God Bless you man. Have a nice day.
Bye
Hey there! This is my first visit to your blog! We are a group of volunteers and starting a new initiative in a community in the same niche.
Your blog provided us valuable information to work on. You have done a
wonderful job!
Club World Cup livescore, FIFA tournament with teams from all continents tracked
日本職棒完整賽程表、戰績排行、即時比分和數據更新。
It’s in point of fact a great and useful piece of info.
I am happy that you simply shared this helpful information with us.
Please keep us informed like this. Thanks for sharing.
It’s amazing to pay a visit this web page and reading the views of all
mates about this piece of writing, while I am also zealous of getting know-how.
Everyone loves it when folks get together and share thoughts.
Great site, keep it up!
QQ88 là nhà cái cá cược uy tín hàng đầu châu Á 2026
QQ88 là nhà cái cá cược uy tín top1 châu Á 2026
qq8876 net thương hiệu cá cược uy tín 2025
qq88 casino là thương hiệu cá cược xanh chín 2025
qq88 agency là thương hiệu cá cược minh bạch 2026
qq88gs.com là nhà cái cá cược minh bạch 2026
QQ88 là nền tảng cá cược trực tuyến uy tín, tích hợp casino live, nổ hũ, bắn cá và thể thao với trải nghiệm ổn định.
Trải nghiệm giải trí online tại QQ88 với kho game đa dạng, giao diện tối ưu và hệ thống vận hành an toàn.
QQ88 là cổng truy cập chính thức giúp người dùng tiếp cận hệ sinh thái giải trí trực tuyến ổn định, giao diện mượt và trải nghiệm an toàn.
Performance live content.
愛壹帆海外版,专为华人打造的高清视频平台采用机器学习个性化推荐,支持全球加速观看。
QQ88 mang đến nền tảng giải trí online được tối ưu tốc độ, giao diện thân thiện và khả năng vận hành ổn định trên nhiều thiết bị.
QQ88 mang đến nền tảng giải trí trực tuyến tối ưu trải nghiệm, chú trọng hiệu quả vận hành và sự thoải mái trong mỗi lần đăng nhập.
Почему пользователи выбирают площадку KRAKEN?
Маркетплейс KRAKEN заслужил доверие многочисленной аудитории благодаря сочетанию ключевых факторов.
Во-первых, это широкий и разнообразный ассортимент, представленный сотнями продавцов.
Во-вторых, интуитивно понятный интерфейс KRAKEN,
который упрощает навигацию, поиск товаров и управление заказами даже
для новых пользователей.
В-третьих, продуманная система безопасных транзакций, включающая механизмы разрешения споров (диспутов) и возможность использования условного депонирования,
что минимизирует риски для обеих сторон сделки.
На KRAKEN функциональность сочетается с внимательным отношением к безопасности клиентов, что
делает процесс покупок более предсказуемым, защищенным
и, как следствие, популярным среди пользователей,
ценящих анонимность и надежность.
QQ88 là cổng truy cập giải trí trực tuyến ổn định, tối ưu tốc độ tải, giao diện mượt và trải nghiệm liền mạch cho người dùng.
QQ88 mang đến nền tảng giải trí trực tuyến được tối ưu toàn diện, chú trọng hiệu quả sử dụng và sự thoải mái khi truy cập.
QQ88 cung cấp môi trường giải trí online hiện đại, dễ thao tác, giao diện mượt và khả năng vận hành ổn định.
QQ88 mang đến cổng truy cập giải trí online hiện đại, tập trung vào hiệu suất, giao diện thân thiện và tính tiện lợi lâu dài.
Почему пользователи выбирают площадку KRAKEN?
Маркетплейс KRAKEN заслужил доверие многочисленной
аудитории благодаря сочетанию ключевых факторов.
Во-первых, это широкий и разнообразный ассортимент, представленный сотнями продавцов.
Во-вторых, интуитивно понятный интерфейс KRAKEN, который упрощает навигацию, поиск товаров и управление заказами даже для
новых пользователей. В-третьих, продуманная система безопасных
транзакций, включающая механизмы разрешения споров (диспутов) и возможность использования условного депонирования,
что минимизирует риски
для обеих сторон сделки. На KRAKEN функциональность сочетается с
внимательным отношением к безопасности
клиентов, что делает процесс покупок более предсказуемым,
защищенным и, как следствие, популярным среди пользователей, ценящих анонимность и надежность.
QQ88 cung cấp môi trường giải trí online hiện đại, tối ưu hiệu suất và đảm bảo trải nghiệm liền mạch khi sử dụng.
It’s perfect time to make some plans for the longer term and it is time to
be happy. I’ve read this submit and if I may I desire to suggest you
some interesting things or tips. Maybe you can write subsequent articles relating to this
article. I wish to read more things approximately it!
thank for sharing
Thanks for Sharing
Great article, very helpful.
The article does a good job explaining
how online cricket streaming works
in a
straightforward format.
Many people often wonder
how they can watch live cricket online
and
this article answers those questions well.
Thanks for sharing.
Really enjoyed reading this post.
It clearly explains
how online cricket streaming works
in a
clear and beginner-friendly manner.
A lot of users are curious
how to access live sports streams
and
this post provides useful insights.
Thanks for putting this together.
This is a very informative post.
The article does a good job explaining
how online cricket streaming works
in a
clear and beginner-friendly manner.
It’s common for readers to ask
how they can watch live cricket online
and
the information here is quite practical.
Thanks for putting this together.
Really enjoyed reading this post.
The article does a good job explaining
how online cricket streaming works
in a
clear and beginner-friendly manner.
Many people often wonder
where to find reliable streaming platforms
and
this article answers those questions well.
Thanks for putting this together.
Hi there, i read your blog occasionally and i own a similar one and i was just curious if you
get a lot of spam responses? If so how do you prevent it, any plugin or anything you can suggest?
I get so much lately it’s driving me mad so any support is very much appreciated.
Great article, very helpful.
It clearly explains
the basics of online sports streaming
in a
straightforward format.
It’s common for readers to ask
where to find reliable streaming platforms
and
the information here is quite practical.
Thanks for putting this together.
I loved as much as you will receive carried out right here.
The sketch is attractive, your authored subject matter stylish.
nonetheless, you command get got an shakiness over that you wish be delivering the following.
unwell unquestionably come further formerly again as exactly the same nearly very often inside case you shield this increase.
Last minute goals, injury time drama and their significance
Риск от наркотиков — это единая хоботня, обхватывающая физическое, психическое равным образом общественное здоровье человека.
Употребление таких наркотиков, как
снежок, мефедрон, гашиш,
«шишки» чи «бошки», что ль огласить
к неконвертируемым последствиям яко чтобы организма, яко (а)
также чтобы среды в течение целом.
Но даже при выковывании связи эвентуально электровосстановление — главное, чтоб зависимый явантроп устремился за помощью.
Важно помнить, что наркомания
врачуется, также восстановление в правах дает шансище
сверху новую жизнь.
Hello There. I found your blog using msn. This is a really well written article.
I’ll be sure to bookmark it and come back to read more
of your useful information. Thanks for the post.
I’ll definitely comeback.
QQ88 MEDIA là thương hiệu cá cược uy tín 2026 kho game đồ sộ thưởng hấp dẫn
I blog frequently and I truly thank you for your information. This article has
really peaked my interest. I’m going to book mark your site and keep checking for new information about once per week.
I opted in for your RSS feed too.
QQ88 trang 1 google.com.vn
Nền tảng giải trí trực tuyến hiện đại, tối ưu trải nghiệm người dùng với tốc độ nhanh, giao diện mượt và vận hành ổn định.
QQ88 LÀ NHÀ CÁI CƯỢC UY TÍN SỐ 1 VN
Live football match score updates faster than TV broadcast, stay ahead of everyone else
Greetings from Colorado! I’m bored to tears
at work so I decided to browse your site on my iphone during lunch break.
I enjoy the info you provide here and can’t wait to take a look when I get home.
I’m amazed at how fast your blog loaded on my mobile ..
I’m not even using WIFI, just 3G .. Anyhow, very good site!
范德沃克高清完整版采用机器学习个性化推荐,海外华人可免费观看最新热播剧集。
QQ88 là cổng truy cập giải trí trực tuyến uy tín, giúp người dùng tiếp cận hệ sinh thái casino, slot, bắn cá và thể thao với giao diện mượt, tốc độ nhanh và trải nghiệm ổn định.
QQ88 là cổng truy cập giải trí trực tuyến ổn định, hỗ trợ người dùng tiếp cận hệ sinh thái game đa dạng với giao diện mượt, tốc độ nhanh và trải nghiệm liền mạch.
This is a very informative post. I really appreciate how clearly everything is explained, especially for people who are new to online casino platforms.
The way you describe the features, usability, and overall experience makes
it easy to understand and compare with other websites.
I also like that the content focuses on safety, convenience, and user experience.
Thanks for sharing such useful information. I will definitely check out more articles on this site.
Thanks for another magnificent article. Where else may anyone get that type of
info in such an ideal manner of writing? I’ve a presentation next week, and I’m at the look for such info.
I have read so many content about the blogger lovers except this post is in fact a fastidious post, keep it
up.
That is a great tip particularly to those fresh
to the blogosphere. Brief but very accurate information…
Many thanks for sharing this one. A must read post!
奥美迦奥特曼高清完整版,海外华人可免费观看最新热播剧集。
QQ88 là nền tảng giải trí trực tuyến được xây dựng nhằm tối ưu trải nghiệm người dùng, hỗ trợ truy cập nhanh, giao diện mượt và khả năng vận hành ổn định trên nhiều thiết bị.
Record breakers, historical milestones and new achievements tracked
This is a very informative post. I really appreciate how clearly everything is explained, especially
for people who are new to online casino platforms.
The way you describe the features, usability, and overall experience makes it easy to understand and compare with other websites.
I also like that the content focuses on safety, convenience, and user
experience.
Thanks for sharing such useful information. I will definitely
check out more articles on this site.
qq88 là nhà cái uy tín số 1 vn mang đến kho game ấn tượng cùng hàn ngàn ưu đãi hấp dẫn
Thanks for the post and great tips..even I also think that hard work is the most important aspect of getting success..
超人和露易斯第二季高清完整版结合大数据AI分析,海外华人可免费观看最新热播剧集。
Pass completion, accuracy rates and distribution statistics tracked
QQ88 là cổng truy cập giải trí trực tuyến uy tín, tối ưu tốc độ, giao diện mượt và mang đến trải nghiệm ổn định cho người dùng.
QQ88 mang đến nền tảng giải trí trực tuyến được tối ưu hiệu suất, giúp người dùng truy cập nhanh, thao tác mượt và trải nghiệm ổn định.
QQ88 là cổng kết nối giải trí online tập trung vào sự ổn định, giao diện thân thiện và trải nghiệm liền mạch.
Bonus veren siteler ile siz de bahis sitelerine para yatırmadan önce deneme bonusu ile siteyi deneyebilirsiniz.
Award winners, individual honors and team trophies documented
QQ88 mang đến cổng truy cập giải trí online hiện đại, chú trọng tốc độ tải, sự thuận tiện và khả năng vận hành liền mạch.
Tennis live scores from all Grand Slams, ATP and WTA tours updated every point
This is a very informative post. I really appreciate how clearly everything is explained, especially for people who are new to
online casino platforms.
The way you describe the features, usability, and overall experience makes it easy to
understand and compare with other websites. I also like that the content focuses
on safety, convenience, and user experience.
Thanks for sharing such useful information. I will definitely check out more articles on this site.
I am regular reader, how are you everybody? This piece of
writing posted at this web page is in fact fastidious.
爱一帆会员多少钱海外版,专为华人打造的高清视频平台,支持全球加速观看。
QQ88 là nền tảng giải trí trực tuyến uy tín, tối ưu tốc độ truy cập, giao diện mượt và trải nghiệm ổn định cho người dùng.
I’m impressed, I have to admit. Seldom do I come across a blog that’s both equally educative and interesting, and without a doubt,
you’ve hit the nail on the head. The problem is an issue that not enough people are
speaking intelligently about. I’m very happy that I stumbled across this during my search
for something regarding this.
QQ88 cung cấp nền tảng giải trí trực tuyến ổn định, tập trung vào tốc độ truy cập, giao diện thân thiện và trải nghiệm liền mạch.
Girişim ekosistemine yaptığınız katkılar için teşekkür ederim. Kişisel gelişim açısından paylaştığınız içerikler çok çok önemli.
Hi, the whole thing is going sound here and ofcourse every one is sharing information, that’s in fact
good, keep up writing.
I’m really inspired together with your writing skills and also with the layout
to your weblog. Is this a paid topic or did you customize it yourself?
Either way stay up the excellent high quality writing, it
is uncommon to see a great weblog like this one today..
Wow, incredible weblog structure! How lengthy have you ever
been blogging for? you made running a blog glance easy. The full glance of your site is excellent, let alone the content material!
If you are going for finest contents like myself, simply pay
a quick visit this web site all the time because
it offers feature contents, thanks
QQ88 là nền tảng giải trí trực tuyến uy tín, tối ưu trải nghiệm với tốc độ truy cập nhanh và giao diện thân thiện.
多瑙高清完整版,海外华人可免费观看最新热播剧集。
塔尔萨之王第二季高清完整版,海外华人可免费观看最新热播剧集。
Hey what a brilliant post I have come across and believe me I have been searching out for this similar kind of post for past a week and hardly came across this. Thank you very much and will look for more postings from you.
QQ88 là thương hiệu cá cược uy tín hàng đầu hiện này mang đến kho game hấp dẫn 2026
QQ88 là nền tảng giải trí trực tuyến uy tín, tối ưu trải nghiệm với tốc độ truy cập nhanh và giao diện thân thiện.
爱亦凡海外版,专为华人打造的高清视频官方认证平台,支持全球加速观看。
爱一帆会员多少钱海外版,专为华人打造的高清视频平台采用机器学习个性化推荐,支持全球加速观看。
QQ88 là cổng truy cập giải trí trực tuyến được tối ưu hiệu suất, giúp người dùng thao tác nhanh và trải nghiệm ổn định.
Interesting article.
The online casino industry in the Philippines continues to evolve quickly, and platforms that
focus on stable systems and transparency tend to stand out.
Consistency and reliability are key factors in long-term success.
We absolutely love your blog and find most of your post’s to be precisely what I’m looking for.
Does one offer guest writers to write content in your case?
I wouldn’t mind publishing a post or elaborating
on many of the subjects you write concerning here.
Again, awesome web log!
QQ88 là nền tảng giải trí trực tuyến uy tín, tối ưu tốc độ truy cập, giao diện mượt và mang lại trải nghiệm ổn định cho người dùng.
Well explained topic.
The online casino industry in the Philippines continues to
grow rapidly, and platforms that focus on security and user experience tend to stand out.
Consistency and reliability are important elements in long-term success.
Good post however , I was wondering if you could write
a litte more on this subject? I’d be very thankful if you could elaborate a little bit more.
Bless you!
QQ88 là cổng truy cập giải trí trực tuyến tối ưu tốc độ, giao diện mượt và mang lại trải nghiệm ổn định cho người dùng.
QQ88 là nền tảng giải trí trực tuyến được tối ưu hiệu suất, giúp người dùng truy cập nhanh và trải nghiệm ổn định.
QQ88 không chỉ là một nền tảng giải trí trực tuyến, mà là không gian được tối ưu trải nghiệm, nơi mọi thao tác đều nhanh, gọn và liền mạch.
Excellent goods from you, man. I have be aware your stuff prior to and you’re
just too wonderful. I really like what you’ve got here, really
like what you’re saying and the way in which wherein you say it.
You’re making it entertaining and you still care for to keep it sensible.
I cant wait to learn much more from you. This is actually a wonderful web site.
Dajemy mu 7 punktów za oryginalność, przyjazny
regulamin, dobry program bonusowy, wspaniałą grafikę i wygodę korzystania.
Hi there! I could have sworn I’ve visited this web
site before but after looking at some of the posts I realized it’s new to me.
Anyhow, I’m definitely delighted I stumbled upon it and I’ll be book-marking it and checking
back often!
Wow, amazing blog layout! How long have you been blogging for?
you make blogging look easy. The overall look of your
website is great, let alone the content!
超人和露易斯第一季高清完整版,海外华人可免费观看最新热播剧集。
huarenus平台,专为海外华人设计,提供高清视频和直播服务。
Giới thiệu với 500 anh em sân chơi xanh chín bậc nhất
mang tên U888. U888 nạp rút siêu tốc độ, không giam tiền. Bác nào chưa thử thì
phí lắm. Cam kết uy tín 100% cho anh em.
Australian online casino real money viva96.com – bonus details
QQ88 được định hình như một không gian giải trí trực tuyến tối ưu hiệu suất, nơi trải nghiệm truy cập nhanh và sự ổn định luôn được đặt lên hàng đầu.
超人和露易斯第一季高清完整官方版,海外华人可免费观看最新热播剧集。
I am actually delighted to glance at this weblog posts which contains tons of helpful data, thanks for providing these kinds of statistics.
夜班医生第四季高清完整版,海外华人可免费观看最新热播剧集。
爱一凡海外版,专为华人打造的高清视频平台,支持全球加速观看。
奇思妙探高清完整官方版,海外华人可免费观看最新热播剧集。
Website của tôi là website chuyên lừa đảo, scam.
Có cả phim sex, phim ấu dâm, phim sex nhật bản
真实的人类第三季高清完整版,海外华人可免费观看最新热播剧集。
iyftv海外华人首选,提供最新华语剧集、美剧、日剧等高清在线观看。
海外华人必备的ifun官方认证平台,24小时不间断提供最新高清电影、电视剧,无广告观看体验。
捕风捉影在线免费在线观看,海外华人专属平台运用AI智能推荐算法,高清无广告体验。
真实的人类第三季高清完整官方版,海外华人可免费观看最新热播剧集。
New online casinos Australia – latest sites with free spins
Top Online Casinos Australia Real Money Including
塔尔萨之王高清完整版,海外华人可免费观看最新热播剧集。
Best pokies online Australia real money – high volatility wins
ifvod平台,专为海外华人设计,提供高清视频和直播服务。
凯伦皮里第二季高清完整版智能AI观看体验优化,海外华人可免费观看最新热播剧集。
官方授权的ifuntv海外华人首选,第一时间提供最新华语剧集、美剧、日剧等高清在线观看。
Australian Online Casino Real Money For Live Baccarat
艾一帆海外版,专为华人打造的高清视频平台AI深度学习内容匹配,支持全球加速观看。
爱一帆会员多少钱海外版,专为华人打造的高清视频平台采用机器学习个性化推荐,支持全球加速观看。
奥美迦奥特曼高清完整版结合大数据AI分析,海外华人可免费观看最新热播剧集。
官方授权的ifuntv海外华人首选,第一时间提供最新华语剧集、美剧、日剧等高清在线观看。
Great blog you have here but I was curious
if you knew of any forums that cover the same topics talked about here?
I’d really love to be a part of online community where I can get feed-back from
other experienced people that share the same interest.
If you have any suggestions, please let me know. Kudos!
爱一帆会员多少钱海外版,专为华人打造的高清视频平台,支持全球加速观看。
What’s up to every body, it’s my first pay a quick visit of this web site; this web
site consists of amazing and genuinely good data for readers.
禁忌第一季高清完整版,海外华人可免费观看最新热播剧集。
Hiya! I know this is kinda off topic however
I’d figured I’d ask. Would you be interested in exchanging links or maybe
guest writing a blog article or vice-versa? My blog goes over a lot of the same
topics as yours and I think we could greatly benefit
from each other. If you are interested feel free to shoot me an e-mail.
I look forward to hearing from you! Terrific blog by the way!
Wow, this post is nice, my younger sister is analyzing these things, thus I am going
to tell her.
Почему пользователи выбирают площадку KRAKEN?
Маркетплейс KRAKEN заслужил доверие многочисленной аудитории благодаря сочетанию ключевых факторов.
Во-первых, это широкий и разнообразный
ассортимент, представленный сотнями продавцов.
Во-вторых, интуитивно понятный интерфейс KRAKEN, который упрощает навигацию, поиск товаров и управление заказами даже для новых пользователей.
В-третьих, продуманная система безопасных
транзакций, включающая механизмы
разрешения споров (диспутов) и возможность использования условного депонирования, что минимизирует риски для обеих сторон сделки.
На KRAKEN функциональность сочетается с внимательным отношением к безопасности клиентов, что делает процесс покупок более предсказуемым,
защищенным и, как следствие, популярным среди пользователей, ценящих анонимность и надежность.
Adelaide United vs Perth Glory – 2026 A-League 16:35 kick-off! Australian football scores & betting buzz live now!
匹兹堡医护前线第二季2026 海外华人免费高清医疗剧 全球加速无广告
Lille 0-1 Crvena Zvezda 2026 Europa League surprise! Red Star shock French side – football news full of underdog glory!
QQ88 là điểm truy cập giải trí trực tuyến được tối ưu toàn diện, tập trung vào tốc độ, sự ổn định và trải nghiệm liền mạch cho người dùng.
Hi to every , because I am really eager of reading this blog’s post to
be updated on a regular basis. It contains good data.
Dinamo Zagreb 1-3 Genk 2026 Europa League score! Belgians dominate – football scores update shows Genk powering through!
QQ88 tạo nên không gian giải trí online linh hoạt, tập trung vào tốc độ, sự liền mạch và cảm giác thoải mái cho người dùng.
逐玉2026 张凌赫田曦薇古装甜宠权谋 海外华人高清在线追剧 全球加速个性化推荐
实习医生风云第十季2026 海外华人医疗喜剧回归 高清经典续集 AI推荐
QQ88 là nền tảng giải trí trực tuyến chú trọng hiệu suất, tối ưu tốc độ truy cập và mang đến trải nghiệm ổn định, liền mạch cho người dùng.
QQ88 là nền tảng giải trí trực tuyến được thiết kế tối giản nhưng hiệu quả, mang đến trải nghiệm truy cập mượt và vận hành ổn định lâu dài
QQ88 định vị mình như một trung tâm giải trí trực tuyến tối ưu trải nghiệm, nơi tốc độ truy cập và sự ổn định luôn được đặt lên hàng đầu.
Почему пользователи выбирают площадку KRAKEN?
Маркетплейс KRAKEN заслужил доверие многочисленной аудитории благодаря сочетанию
ключевых факторов. Во-первых, это широкий и разнообразный ассортимент, представленный
сотнями продавцов. Во-вторых, интуитивно понятный интерфейс KRAKEN,
который упрощает навигацию, поиск товаров и управление заказами даже для новых пользователей.
В-третьих, продуманная система безопасных транзакций, включающая механизмы разрешения споров (диспутов) и возможность использования условного депонирования, что минимизирует
риски для обеих сторон сделки.
На KRAKEN функциональность сочетается с внимательным отношением к безопасности клиентов, что делает процесс покупок более предсказуемым, защищенным и,
как следствие, популярным
среди пользователей, ценящих анонимность
и надежность.
I really like your blog.. very nice colors & theme. Did you create
this website yourself or did you hire someone to do it for you?
Plz reply as I’m looking to construct my own blog
and would like to know where u got this from. thanks a lot
QQ88 là không gian giải trí trực tuyến được tối ưu trải nghiệm, nơi tốc độ, sự ổn định và tính tiện lợi được đặt lên hàng đầu.
I was very happy to find this site. I want to to thank you for your
time due to this wonderful read!! I definitely savored
every bit of it and i also have you bookmarked to check
out new stuff on your website.
Wow, incredible blog layout! How long have you been blogging
for? you make blogging look easy. The overall look of your website is fantastic, as
well as the content!
You’re so cool! I don’t think I’ve read through a single thing like that before.
So great to discover another person with original thoughts on this subject matter.
Seriously.. thank you for starting this up. This web site is one thing that is required on the
internet, someone with a little originality!
I am actually glad to read this weblog posts which includes
plenty of valuable information, thanks for providing
these kinds of information.
Everyone loves it whenever people get together and share views.
Great site, continue the good work!
Having read this I believed it was really enlightening. I appreciate you spending
some time and effort to put this article together.
I once again find myself spending way too much time both reading and posting comments.
But so what, it was still worthwhile!
I like it when folks get together and share opinions. Great site, keep it up!
逐玉2026 张凌赫田曦薇 高清古装甜宠权谋 海外华人高清在线 全球加速AI推荐
QQ88 mang đến hệ sinh thái giải trí toàn diện: cược thể thao, live casino, slot nổ hũ, đá gà, xổ số. Tốc độ mượt, giao dịch nhanh, hỗ trợ 24/7.
QQ88 khẳng định đẳng cấp với hệ thống cá cược hiện đại, tỷ lệ kèo hấp dẫn, thưởng minh bạch. Trải nghiệm mượt mà trên mọi thiết bị, hỗ trợ tận tâm 24/7.
What’s Going down i am new to this, I stumbled upon this I’ve discovered It
absolutely helpful and it has aided me out loads.
I’m hoping to give a contribution & aid other users like its helped me.
Great job.
Yay google is my world beater assisted me to find this great internet site!
Brest vs Marseille – 2026 Ligue 1 blockbuster 20:45! Can Marseille steal points on the road? French football latest match results incoming!
Greetings! I know this is kind of off topic but I was wondering if you knew
where I could locate a captcha plugin for my comment form?
I’m using the same blog platform as yours and I’m having difficulty finding one?
Thanks a lot!
QQ88 – Hệ sinh thái cá cược trực tuyến toàn diện, tích hợp Thể thao, Live Casino, Slot nổ hũ và Bắn cá đổi thưởng. Giao diện hiện đại, tốc độ xử lý nhanh, trải nghiệm ổn định.
QQ88 – Thương hiệu cá cược trực tuyến uy tín, hội tụ đầy đủ Thể thao, Casino live, Slot nổ hũ, Bắn cá và Đá gà. Trải nghiệm mượt mà, thưởng minh bạch, hỗ trợ 24/7.
QQ88 – Cổng game cá cược trực tuyến quy tụ hàng triệu thành viên, nổi bật với Thể thao, Live Casino, Slot nổ hũ và Bắn cá đổi thưởng. Giao diện tối ưu, chơi mượt trên mọi nền tảng.
QQ88 – Điểm hẹn cá cược trực tuyến đẳng cấp với kho trò chơi đa dạng: Thể thao, Casino live, Nổ hũ, Bắn cá, Xổ số. Trải nghiệm ổn định, giao dịch nhanh, ưu đãi liên tục.
QQ88 – Nền tảng cá cược trực tuyến uy tín với hệ sinh thái Thể thao, Casino live, Slot nổ hũ, Bắn cá và Đá gà. Trải nghiệm mượt mà, tỷ lệ kèo hấp dẫn, ưu đãi mỗi ngày.
QQ88 – Cổng game cá cược trực tuyến nổi bật với kho trò chơi phong phú: Thể thao, Live Casino, Nổ hũ, Bắn cá, Xổ số. Nạp rút nhanh, bảo mật cao, trải nghiệm mượt mà.
QQ88 là điểm đến quen thuộc của cộng đồng bet thủ nhờ hệ thống minh bạch, kèo cược cạnh tranh và trải nghiệm mượt trên mọi thiết bị. Hỗ trợ 24/7, chơi là mê.
I do accept as true with all the ideas you have presented on your post.
They’re really convincing and will definitely work. Nonetheless, the posts are very short for beginners.
May just you please lengthen them a little from next time?
Thanks for the post.
qq88 là nhà cái uy tín hàngđầu châu á, mang đến kho game hấp dẫn 2026
(10 euros gratis apuestas|10 mejores casas de apuestas|10 trucos para ganar apuestas|15 euros gratis marca apuestas|1×2 apuestas|1×2 apuestas
deportivas|1×2 apuestas que significa|1×2 en apuestas|1×2 en apuestas que significa|1×2
que significa en apuestas|5 euros gratis apuestas|9 apuestas que siempre ganaras|a partir de cuanto se declara
apuestas|actividades de juegos de azar y apuestas|ad apuestas deportivas|aleksandre topuria ufc apuestas|algoritmo para ganar apuestas deportivas|america apuestas|análisis nba apuestas|aplicacion android apuestas deportivas|aplicacion apuestas deportivas|aplicacion apuestas deportivas android|aplicación de apuestas
online|aplicacion para hacer apuestas|aplicacion para hacer apuestas de
futbol|aplicación para hacer apuestas de fútbol|aplicaciones apuestas deportivas android|aplicaciones apuestas deportivas gratis|aplicaciones de
apuestas android|aplicaciones de apuestas de fútbol|aplicaciones de apuestas deportivas|aplicaciones de apuestas deportivas peru|aplicaciones de apuestas deportivas perú|aplicaciones de apuestas en colombia|aplicaciones de apuestas gratis|aplicaciones de apuestas online|aplicaciones de apuestas seguras|aplicaciones de apuestas sin dinero|aplicaciones para hacer apuestas|apostar seguro apuestas deportivas|app android
apuestas deportivas|app apuestas|app apuestas android|app
apuestas de futbol|app apuestas deportivas|app apuestas deportivas android|app apuestas deportivas argentina|app apuestas deportivas colombia|app
apuestas deportivas ecuador|app apuestas deportivas españa|app apuestas deportivas gratis|app apuestas entre amigos|app apuestas futbol|app apuestas gratis|app
apuestas sin dinero|app casa de apuestas|app casas de apuestas|app control apuestas|app de apuestas|app de
apuestas android|app de apuestas casino|app de apuestas colombia|app de apuestas con bono de
bienvenida|app de apuestas de futbol|app de apuestas deportivas|app de apuestas deportivas
android|app de apuestas deportivas argentina|app de apuestas deportivas colombia|app de
apuestas deportivas en españa|app de apuestas deportivas peru|app de apuestas deportivas perú|app de apuestas deportivas sin dinero|app de apuestas ecuador|app de
apuestas en colombia|app de apuestas en españa|app de apuestas
en venezuela|app de apuestas futbol|app de apuestas gratis|app de apuestas online|app de
apuestas para android|app de apuestas para ganar dinero|app
de apuestas peru|app de apuestas reales|app de casas de apuestas|app marca
apuestas android|app moviles de apuestas|app para apuestas|app para apuestas de futbol|app para apuestas
deportivas|app para apuestas deportivas en español|app para ganar apuestas deportivas|app para hacer
apuestas|app para hacer apuestas deportivas|app para hacer
apuestas entre amigos|app para llevar control de apuestas|app pronosticos apuestas deportivas|app versus apuestas|apps apuestas mundial|apps de apuestas|apps
de apuestas con bono de bienvenida|apps de apuestas de futbol|apps de apuestas deportivas peru|apps de apuestas mexico|apps para apuestas|aprender
a hacer apuestas deportivas|aprender hacer apuestas deportivas|apuesta
del dia apuestas deportivas|apuestas 10 euros gratis|apuestas 100 seguras|apuestas 1×2|apuestas 1X2|apuestas
2 division|apuestas 3 division|apuestas a caballos|apuestas a carreras de caballos|apuestas a colombia|apuestas a corners|apuestas a ganar|apuestas a jugadores nba|apuestas
a la baja|apuestas a la nfl|apuestas al barcelona|apuestas al dia|apuestas al
empate|apuestas al mundial|apuestas al tenis wta|apuestas alaves barcelona|apuestas alcaraz hoy|apuestas alemania españa|apuestas alonso campeon del
mundo|apuestas altas y bajas|apuestas altas y bajas nfl|apuestas ambos equipos marcan|apuestas america|apuestas android|apuestas anillo nba|apuestas antes del
mundial|apuestas anticipadas|apuestas anticipadas nba|apuestas
apps|apuestas arabia argentina|apuestas argentina|apuestas argentina campeon del mundo|apuestas argentina canada|apuestas argentina colombia|apuestas argentina
croacia|apuestas argentina españa|apuestas argentina francia|apuestas
argentina francia cuanto paga|apuestas argentina francia mundial|apuestas argentina
gana el mundial|apuestas argentina gana mundial|apuestas argentina holanda|apuestas
argentina mexico|apuestas argentina méxico|apuestas
argentina mundial|apuestas argentina online|apuestas argentina paises bajos|apuestas argentina
polonia|apuestas argentina uruguay|apuestas argentina vs australia|apuestas argentina vs colombia|apuestas argentina vs francia|apuestas argentina vs peru|apuestas argentinas|apuestas arsenal real madrid|apuestas ascenso a
primera division|apuestas ascenso a segunda|apuestas
asiaticas|apuestas asiatico|apuestas athletic|apuestas athletic atletico|apuestas athletic barça|apuestas athletic barcelona|apuestas athletic betis|apuestas athletic manchester|apuestas athletic manchester united|apuestas athletic osasuna|apuestas athletic real|apuestas athletic real madrid|apuestas athletic real sociedad|apuestas athletic real sociedad
final|apuestas athletic roma|apuestas athletic sevilla|apuestas
athletic valencia|apuestas atletico|apuestas atletico barcelona|apuestas atletico
barsa|apuestas atletico campeon champions|apuestas atletico campeon de liga|apuestas atlético copenhague|apuestas atletico de madrid|apuestas
atlético de madrid|apuestas atletico de madrid barcelona|apuestas atletico de
madrid gana la liga|apuestas atletico de madrid real madrid|apuestas atlético de madrid real
madrid|apuestas atletico de madrid vs barcelona|apuestas atletico madrid|apuestas atletico madrid real madrid|apuestas atletico madrid vs barcelona|apuestas atletico real madrid|apuestas atletico real madrid
champions|apuestas atletismo|apuestas bajas|apuestas baloncesto|apuestas
baloncesto acb|apuestas baloncesto handicap|apuestas baloncesto hoy|apuestas
baloncesto juegos olimpicos|apuestas baloncesto nba|apuestas baloncesto
pronostico|apuestas baloncesto pronósticos|apuestas baloncesto prorroga|apuestas
barca|apuestas barca athletic|apuestas barca atletico|apuestas barca bayern|apuestas barca bayern munich|apuestas barca girona|apuestas barca
hoy|apuestas barça hoy|apuestas barca inter|apuestas
barca juventus|apuestas barca madrid|apuestas barça madrid|apuestas barca
real madrid|apuestas barca vs juve|apuestas barca vs madrid|apuestas barca vs psg|apuestas
barcelona|apuestas barcelona alaves|apuestas barcelona athletic|apuestas
barcelona atletico|apuestas barcelona atletico de madrid|apuestas barcelona atlético de madrid|apuestas barcelona atletico madrid|apuestas barcelona bayern|apuestas barcelona betis|apuestas barcelona campeon de liga|apuestas barcelona celta|apuestas barcelona espanyol|apuestas barcelona gana la champions|apuestas
barcelona girona|apuestas barcelona granada|apuestas barcelona hoy|apuestas barcelona
inter|apuestas barcelona madrid|apuestas barcelona osasuna|apuestas barcelona psg|apuestas
barcelona real madrid|apuestas barcelona real sociedad|apuestas barcelona sevilla|apuestas barcelona valencia|apuestas barcelona villarreal|apuestas barcelona vs atletico madrid|apuestas barcelona vs madrid|apuestas barcelona vs
real madrid|apuestas barsa madrid|apuestas basket hoy|apuestas
bayern barcelona|apuestas bayern vs barcelona|apuestas beisbol|apuestas béisbol|apuestas beisbol mlb|apuestas
beisbol pronosticos|apuestas beisbol venezolano|apuestas
betis|apuestas betis – chelsea|apuestas betis barcelona|apuestas betis chelsea|apuestas
betis fiorentina|apuestas betis girona|apuestas betis madrid|apuestas betis mallorca|apuestas betis real madrid|apuestas
betis real sociedad|apuestas betis sevilla|apuestas betis valencia|apuestas betis valladolid|apuestas
betis vs valencia|apuestas betplay hoy colombia|apuestas betsson peru|apuestas bienvenida|apuestas billar online|apuestas bolivia vs colombia|apuestas bono|apuestas
bono bienvenida|apuestas bono de bienvenida|apuestas bono
de bienvenida sin deposito|apuestas bono gratis|apuestas bono sin deposito|apuestas bonos
sin deposito|apuestas borussia real madrid|apuestas boxeo|apuestas boxeo de
campeonato|apuestas boxeo españa|apuestas boxeo español|apuestas boxeo femenino olimpiadas|apuestas boxeo hoy|apuestas boxeo online|apuestas brasil
colombia|apuestas brasil peru|apuestas brasil
uruguay|apuestas brasil vs colombia|apuestas brasil vs peru|apuestas caballos|apuestas caballos
colocado|apuestas caballos españa|apuestas caballos
hipodromo|apuestas caballos hoy|apuestas caballos madrid|apuestas caballos
online|apuestas caballos sanlucar de barrameda|apuestas
caballos zarzuela|apuestas calculador|apuestas campeon|apuestas campeon champions|apuestas campeón champions|apuestas campeon champions
2025|apuestas campeon champions league|apuestas campeon conference league|apuestas campeon copa america|apuestas campeon copa del rey|apuestas campeon de champions|apuestas campeon de la champions|apuestas campeon de liga|apuestas campeon del mundo|apuestas campeon eurocopa|apuestas
campeón eurocopa|apuestas campeon europa league|apuestas campeon f1|apuestas campeon f1
2025|apuestas campeon formula 1|apuestas campeon libertadores|apuestas campeon liga|apuestas campeon liga bbva|apuestas campeon liga
española|apuestas campeon liga santander|apuestas campeon motogp 2025|apuestas campeon mundial|apuestas campeón mundial|apuestas campeon mundial baloncesto|apuestas campeon nba|apuestas campeón nba|apuestas
campeon premier|apuestas campeon premier league|apuestas campeon roland garros|apuestas campeonato f1|apuestas campeonatos de futbol|apuestas carrera
de caballos|apuestas carrera de caballos hoy|apuestas carrera de
caballos nocturnas|apuestas carrera de galgos fin de semana|apuestas carrera de
galgos hoy|apuestas carrera de galgos nocturnas|apuestas carreras caballos|apuestas carreras caballos
sanlucar|apuestas carreras de caballos|apuestas carreras de
caballos en directo|apuestas carreras de caballos en vivo|apuestas carreras de caballos españa|apuestas carreras de caballos hoy|apuestas carreras de caballos nacionales|apuestas carreras de caballos nocturnas|apuestas carreras de caballos online|apuestas carreras de caballos sanlucar|apuestas carreras de caballos sanlúcar|apuestas carreras de galgos|apuestas carreras
de galgos en vivo|apuestas carreras de galgos nocturnas|apuestas carreras de galgos pre partido|apuestas casino|apuestas
casino barcelona|apuestas casino futbol|apuestas casino gran madrid|apuestas
casino gratis|apuestas casino madrid|apuestas casino
online|apuestas casino online argentina|apuestas casinos|apuestas casinos online|apuestas celta|apuestas celta
barcelona|apuestas celta betis|apuestas celta eibar|apuestas celta espanyol|apuestas celta granada|apuestas celta madrid|apuestas
celta manchester|apuestas celta real madrid|apuestas champion league|apuestas champions foro|apuestas
champions hoy|apuestas champions league|apuestas champions league
– pronósticos|apuestas champions league 2025|apuestas champions
league hoy|apuestas champions league pronosticos|apuestas champions league pronósticos|apuestas champions pronosticos|apuestas chelsea barcelona|apuestas chelsea betis|apuestas chile|apuestas chile peru|apuestas chile venezuela|apuestas chile vs colombia|apuestas chile vs
uruguay|apuestas ciclismo|apuestas ciclismo en vivo|apuestas ciclismo femenino|apuestas ciclismo tour francia|apuestas
ciclismo vuelta|apuestas ciclismo vuelta a españa|apuestas ciclismo vuelta españa|apuestas city madrid|apuestas city
real madrid|apuestas clasico|apuestas clasico español|apuestas clasico real madrid barcelona|apuestas clasificacion mundial|apuestas colombia|apuestas colombia argentina|apuestas colombia brasil|apuestas colombia paraguay|apuestas colombia uruguay|apuestas colombia vs argentina|apuestas colombia vs
brasil|apuestas combinadas|apuestas combinadas como funcionan|apuestas combinadas de futbol|apuestas combinadas de fútbol|apuestas combinadas foro|apuestas combinadas futbol|apuestas combinadas hoy|apuestas combinadas
mismo partido|apuestas combinadas mundial|apuestas combinadas nba|apuestas combinadas para esta semana|apuestas combinadas
para hoy|apuestas combinadas para mañana|apuestas combinadas
pronosticos|apuestas combinadas recomendadas|apuestas combinadas seguras|apuestas combinadas seguras
para hoy|apuestas combinadas seguras para mañana|apuestas como ganar|apuestas comparador|apuestas con bono
de bienvenida|apuestas con dinero ficticio|apuestas con dinero
real|apuestas con dinero virtual|apuestas con handicap|apuestas con handicap asiatico|apuestas con handicap baloncesto|apuestas con mas probabilidades de ganar|apuestas con paypal|apuestas
con tarjeta de credito|apuestas con tarjeta de debito|apuestas consejos|apuestas copa|apuestas copa africa|apuestas copa america|apuestas copa
américa|apuestas copa argentina|apuestas copa brasil|apuestas copa davis|apuestas copa de europa|apuestas copa del mundo|apuestas
copa del rey|apuestas copa del rey baloncesto|apuestas
copa del rey final|apuestas copa del rey futbol|apuestas copa del rey ganador|apuestas copa del rey hoy|apuestas copa del rey pronosticos|apuestas copa del rey pronósticos|apuestas copa europa|apuestas copa italia|apuestas copa libertadores|apuestas
copa mundial de hockey|apuestas copa rey|apuestas copa sudamericana|apuestas corners|apuestas corners hoy|apuestas croacia argentina|apuestas cuartos
eurocopa|apuestas cuotas|apuestas cuotas altas|apuestas
cuotas bajas|apuestas de 1 euro|apuestas de
baloncesto|apuestas de baloncesto hoy|apuestas de baloncesto nba|apuestas de baloncesto para hoy|apuestas
de beisbol|apuestas de beisbol para hoy|apuestas de blackjack en linea|apuestas de boxeo|apuestas de boxeo canelo|apuestas de boxeo en las
vegas|apuestas de boxeo hoy|apuestas de boxeo online|apuestas de caballo|apuestas
de caballos|apuestas de caballos como funciona|apuestas de caballos como se juega|apuestas de caballos en colombia|apuestas de caballos en españa|apuestas de caballos
en linea|apuestas de caballos españa|apuestas de caballos ganador y colocado|apuestas de caballos internacionales|apuestas de caballos juegos|apuestas de caballos online|apuestas
de caballos online en venezuela|apuestas de caballos por internet|apuestas de caballos pronosticos|apuestas de caballos pronósticos|apuestas de carrera de caballos|apuestas de
carreras de caballos|apuestas de carreras de caballos online|apuestas de casino|apuestas de casino online|apuestas de
casino por internet|apuestas de champions league|apuestas de ciclismo|apuestas de colombia|apuestas de copa america|apuestas de corners|apuestas de deportes en linea|apuestas de
deportes online|apuestas de dinero|apuestas de esports|apuestas de eurocopa|apuestas de europa league|apuestas de f1|apuestas de
formula 1|apuestas de futbol|apuestas de fútbol|apuestas de
futbol app|apuestas de futbol argentina|apuestas de futbol colombia|apuestas
de futbol en colombia|apuestas de futbol en directo|apuestas de futbol
en linea|apuestas de futbol en vivo|apuestas de futbol español|apuestas de futbol gratis|apuestas de futbol hoy|apuestas
de futbol mundial|apuestas de futbol online|apuestas de fútbol
online|apuestas de futbol para hoy|apuestas de fútbol para hoy|apuestas de futbol para hoy seguras|apuestas de futbol para mañana|apuestas de futbol peru|apuestas de futbol pronosticos|apuestas de fútbol
pronósticos|apuestas de futbol seguras|apuestas de futbol seguras para hoy|apuestas de futbol sin dinero|apuestas de galgos|apuestas
de galgos como ganar|apuestas de galgos en directo|apuestas
de galgos online|apuestas de galgos trucos|apuestas de golf|apuestas de hockey|apuestas
de hockey sobre hielo|apuestas de hoy|apuestas de hoy seguras|apuestas de juego|apuestas de juegos|apuestas de juegos deportivos|apuestas de juegos online|apuestas de la champions league|apuestas de la copa
américa|apuestas de la eurocopa|apuestas de la europa league|apuestas de la
liga|apuestas de la liga bbva|apuestas de la liga
española|apuestas de la nba|apuestas de la nfl|apuestas de la ufc|apuestas
de mlb|apuestas de nba|apuestas de nba para hoy|apuestas de partidos|apuestas de partidos de futbol|apuestas de peleas
ufc|apuestas de perros en vivo|apuestas de perros virtuales|apuestas de peru|apuestas de
sistema|apuestas de sistema como funciona|apuestas de sistema explicacion|apuestas de sistema explicación|apuestas de tenis|apuestas de tenis de mesa|apuestas de tenis en directo|apuestas de tenis hoy|apuestas de
tenis para hoy|apuestas de tenis pronosticos|apuestas
de tenis seguras|apuestas de todo tipo|apuestas de ufc|apuestas
de ufc hoy|apuestas del boxeo|apuestas del clasico|apuestas del clasico real madrid barca|apuestas del dia|apuestas del día|apuestas del dia de hoy|apuestas del dia deportivas|apuestas del dia
futbol|apuestas del mundial|apuestas del partido de hoy|apuestas
del real madrid|apuestas del rey|apuestas del sistema|apuestas
deporte|apuestas deportes|apuestas deportiva|apuestas deportivas|apuestas deportivas 1 euro|apuestas
deportivas 10 euros gratis|apuestas deportivas 100
seguras|apuestas deportivas 1×2|apuestas deportivas
android|apuestas deportivas app|apuestas deportivas apps|apuestas deportivas argentina|apuestas deportivas argentina futbol|apuestas deportivas argentina
legal|apuestas deportivas atletico de madrid|apuestas deportivas
baloncesto|apuestas deportivas barca madrid|apuestas deportivas
barcelona|apuestas deportivas beisbol|apuestas deportivas bono|apuestas deportivas bono bienvenida|apuestas deportivas bono de bienvenida|apuestas deportivas
bono sin deposito|apuestas deportivas bonos de bienvenida|apuestas deportivas
boxeo|apuestas deportivas caballos|apuestas deportivas
calculadora|apuestas deportivas campeon liga|apuestas deportivas casino|apuestas deportivas casino barcelona|apuestas deportivas casino online|apuestas deportivas cerca de mi|apuestas deportivas champions league|apuestas deportivas chile|apuestas deportivas ciclismo|apuestas deportivas colombia|apuestas deportivas com|apuestas
deportivas com foro|apuestas deportivas com pronosticos|apuestas deportivas combinadas|apuestas deportivas combinadas para hoy|apuestas
deportivas como se juega|apuestas deportivas comparador|apuestas deportivas con bono gratis|apuestas
deportivas con bonos gratis|apuestas deportivas con dinero ficticio|apuestas deportivas con paypal|apuestas
deportivas con puntos virtuales|apuestas deportivas consejos|apuestas deportivas
consejos para ganar|apuestas deportivas copa america|apuestas deportivas copa del rey|apuestas deportivas copa libertadores|apuestas deportivas copa mundial|apuestas deportivas corners|apuestas deportivas cual es la mejor|apuestas
deportivas cuotas altas|apuestas deportivas de baloncesto|apuestas deportivas de boxeo|apuestas
deportivas de colombia|apuestas deportivas de futbol|apuestas
deportivas de nba|apuestas deportivas de nhl|apuestas deportivas
de peru|apuestas deportivas de tenis|apuestas deportivas del dia|apuestas deportivas dinero ficticio|apuestas deportivas directo|apuestas deportivas doble oportunidad|apuestas deportivas en argentina|apuestas deportivas en chile|apuestas deportivas en colombia|apuestas deportivas en directo|apuestas deportivas en españa|apuestas deportivas en español|apuestas deportivas en linea|apuestas deportivas
en línea|apuestas deportivas en peru|apuestas deportivas en perú|apuestas deportivas en sevilla|apuestas deportivas en uruguay|apuestas deportivas en vivo|apuestas deportivas es|apuestas deportivas es pronosticos|apuestas deportivas
españa|apuestas deportivas españolas|apuestas deportivas esports|apuestas deportivas estadisticas|apuestas deportivas estrategias|apuestas deportivas estrategias seguras|apuestas deportivas
eurocopa|apuestas deportivas europa league|apuestas deportivas
f1|apuestas deportivas faciles de ganar|apuestas deportivas
formula 1|apuestas deportivas foro|apuestas
deportivas foro futbol|apuestas deportivas foro tenis|apuestas deportivas francia argentina|apuestas deportivas futbol|apuestas deportivas fútbol|apuestas deportivas futbol argentino|apuestas deportivas futbol
colombia|apuestas deportivas futbol español|apuestas deportivas gana|apuestas deportivas ganadas|apuestas deportivas ganar dinero seguro|apuestas deportivas gane|apuestas deportivas golf|apuestas deportivas
gratis|apuestas deportivas gratis con premios|apuestas deportivas gratis
hoy|apuestas deportivas gratis sin deposito|apuestas deportivas handicap|apuestas deportivas handicap asiatico|apuestas deportivas hoy|apuestas deportivas impuestos|apuestas
deportivas interior argentina|apuestas deportivas juegos olimpicos|apuestas deportivas la liga|apuestas deportivas legales|apuestas deportivas legales en colombia|apuestas deportivas libres de impuestos|apuestas
deportivas licencia españa|apuestas deportivas liga española|apuestas deportivas listado|apuestas deportivas listado clasico|apuestas deportivas madrid|apuestas deportivas mas seguras|apuestas deportivas
mejor pagadas|apuestas deportivas mejores|apuestas deportivas mejores app|apuestas deportivas
mejores casas|apuestas deportivas mejores cuotas|apuestas deportivas mejores paginas|apuestas
deportivas mexico|apuestas deportivas méxico|apuestas deportivas mlb|apuestas deportivas mlb hoy|apuestas
deportivas multiples|apuestas deportivas mundial|apuestas deportivas murcia|apuestas
deportivas nba|apuestas deportivas nba hoy|apuestas deportivas nfl|apuestas deportivas nhl|apuestas deportivas nuevas|apuestas deportivas ofertas|apuestas deportivas
online|apuestas deportivas online argentina|apuestas deportivas online chile|apuestas deportivas online colombia|apuestas deportivas online en colombia|apuestas deportivas online españa|apuestas deportivas online mexico|apuestas deportivas online paypal|apuestas deportivas online peru|apuestas deportivas online por internet|apuestas deportivas pago paypal|apuestas deportivas para ganar dinero|apuestas deportivas
para hoy|apuestas deportivas para hoy pronosticos|apuestas deportivas partido suspendido|apuestas
deportivas partidos de hoy|apuestas deportivas paypal|apuestas deportivas peru|apuestas deportivas perú|apuestas deportivas peru vs ecuador|apuestas deportivas predicciones|apuestas deportivas promociones|apuestas deportivas pronostico|apuestas deportivas pronóstico|apuestas
deportivas pronostico hoy|apuestas deportivas pronosticos|apuestas
deportivas pronósticos|apuestas deportivas pronosticos expertos|apuestas deportivas pronosticos gratis|apuestas deportivas pronosticos nba|apuestas deportivas
pronosticos tenis|apuestas deportivas que aceptan paypal|apuestas deportivas real madrid|apuestas deportivas regalo bienvenida|apuestas deportivas resultado exacto|apuestas deportivas resultados|apuestas deportivas rugby|apuestas deportivas seguras|apuestas deportivas seguras foro|apuestas deportivas seguras hoy|apuestas deportivas seguras para hoy|apuestas deportivas
seguras telegram|apuestas deportivas sevilla|apuestas deportivas simulador eurocopa|apuestas deportivas sin deposito|apuestas deportivas sin deposito inicial|apuestas deportivas sin dinero|apuestas deportivas sin dinero
real|apuestas deportivas sin registro|apuestas deportivas stake|apuestas deportivas stake
10|apuestas deportivas telegram españa|apuestas deportivas tenis|apuestas deportivas tenis de mesa|apuestas deportivas tenis
foro|apuestas deportivas tenis hoy|apuestas deportivas
tips|apuestas deportivas tipster|apuestas deportivas ufc|apuestas deportivas uruguay|apuestas deportivas
valencia|apuestas deportivas valencia barcelona|apuestas deportivas venezuela|apuestas deportivas virtuales|apuestas deportivas
y casino|apuestas deportivas y casino online|apuestas
deportivas.com|apuestas deportivas.com foro|apuestas deportivas.es|apuestas
deportivos pronosticos|apuestas deposito minimo 1 euro|apuestas descenso a segunda|apuestas descenso a segunda b|apuestas descenso la liga|apuestas descenso
primera division|apuestas descenso segunda|apuestas dia|apuestas diarias
seguras|apuestas dinero|apuestas dinero ficticio|apuestas
dinero real|apuestas dinero virtual|apuestas directas|apuestas directo|apuestas directo futbol|apuestas division de
honor juvenil|apuestas dnb|apuestas doble oportunidad|apuestas doble resultado|apuestas dobles|apuestas dobles y triples|apuestas dortmund barcelona|apuestas draft nba|apuestas draft nfl|apuestas ecuador vs argentina|apuestas ecuador vs
venezuela|apuestas egipto uruguay|apuestas el clasico|apuestas elecciones venezuela|apuestas
empate|apuestas en baloncesto|apuestas en barcelona|apuestas en beisbol|apuestas en boxeo|apuestas en caballos|apuestas en carreras de caballos|apuestas en casino|apuestas en casino online|apuestas en casinos|apuestas en casinos
online|apuestas en chile|apuestas en ciclismo|apuestas en colombia|apuestas en colombia de futbol|apuestas en directo|apuestas en directo futbol|apuestas en directo pronosticos|apuestas en el futbol|apuestas en el tenis|apuestas en españa|apuestas en esports|apuestas en eventos deportivos virtuales|apuestas en golf|apuestas en juegos|apuestas en la champions league|apuestas en la eurocopa|apuestas en la liga|apuestas en la nba|apuestas en la nfl|apuestas en las
vegas mlb|apuestas en las vegas nfl|apuestas en linea|apuestas en línea|apuestas en linea argentina|apuestas en linea boxeo|apuestas en linea chile|apuestas en linea colombia|apuestas en línea de fútbol|apuestas en linea deportivas|apuestas en linea españa|apuestas en linea estados unidos|apuestas en linea
futbol|apuestas en linea mexico|apuestas en línea méxico|apuestas en linea mundial|apuestas en linea peru|apuestas en linea usa|apuestas en los esports|apuestas en madrid|apuestas en méxico|apuestas en mexico online|apuestas en nba|apuestas en partidos
de futbol|apuestas en partidos de futbol en vivo|apuestas en partidos de tenis en directo|apuestas en perú|apuestas en sevilla|apuestas en sistema|apuestas en stake|apuestas en tenis|apuestas en tenis de
mesa|apuestas en valencia|apuestas en vivo|apuestas en vivo argentina|apuestas
en vivo casino|apuestas en vivo futbol|apuestas en vivo fútbol|apuestas en vivo nba|apuestas en vivo peru|apuestas en vivo tenis|apuestas en vivo
ufc|apuestas equipo mbappe|apuestas equipos de futbol|apuestas españa|apuestas españa alemania|apuestas españa alemania eurocopa|apuestas
españa croacia|apuestas españa eurocopa|apuestas españa francia|apuestas españa francia eurocopa|apuestas españa gana el mundial|apuestas españa gana eurocopa|apuestas españa gana mundial|apuestas españa georgia|apuestas españa holanda|apuestas españa inglaterra|apuestas
españa inglaterra cuotas|apuestas españa inglaterra eurocopa|apuestas
españa italia|apuestas españa mundial|apuestas españa paises bajos|apuestas español|apuestas español
oviedo|apuestas espanyol barcelona|apuestas espanyol betis|apuestas espanyol villarreal|apuestas esport|apuestas esports|apuestas esports colombia|apuestas esports españa|apuestas esports
fifa|apuestas esports gratis|apuestas esports lol|apuestas esports peru|apuestas esports
valorant|apuestas estadisticas|apuestas estrategias|apuestas euro|apuestas euro copa|apuestas eurocopa|apuestas eurocopa
campeon|apuestas eurocopa españa|apuestas eurocopa favoritos|apuestas eurocopa femenina|apuestas eurocopa final|apuestas eurocopa ganador|apuestas eurocopa
hoy|apuestas eurocopa sub 21|apuestas euroliga baloncesto|apuestas euroliga pronosticos|apuestas europa league|apuestas europa league hoy|apuestas europa league pronosticos|apuestas
europa league pronósticos|apuestas euros|apuestas f1 abu dhabi|apuestas f1 bahrein|apuestas f1 canada|apuestas f1 china|apuestas f1 cuotas|apuestas f1 hoy|apuestas f1 las vegas|apuestas f1 miami|apuestas
f1 monaco|apuestas faciles de ganar|apuestas fáciles de ganar|apuestas faciles para ganar|apuestas favoritas|apuestas favorito champions|apuestas favoritos champions|apuestas favoritos eurocopa|apuestas favoritos mundial|apuestas fc barcelona|apuestas final champions cuotas|apuestas final
champions league|apuestas final champions peru|apuestas final copa|apuestas
final copa america|apuestas final copa de europa|apuestas final copa del rey|apuestas final copa europa|apuestas final copa
libertadores|apuestas final copa rey|apuestas final de copa|apuestas
final de copa del rey|apuestas final del mundial|apuestas final euro|apuestas final eurocopa|apuestas final europa league|apuestas
final libertadores|apuestas final mundial|apuestas final nba|apuestas final rugby|apuestas final uefa europa
league|apuestas final.mundial|apuestas finales de conferencia nfl|apuestas finales nba|apuestas fiorentina betis|apuestas
formula|apuestas formula 1|apuestas fórmula 1|apuestas fórmula 1
pronósticos|apuestas formula uno|apuestas foro|apuestas foro nba|apuestas francia argentina|apuestas francia españa|apuestas futbol|apuestas fútbol|apuestas futbol americano|apuestas
futbol americano nfl|apuestas futbol argentina|apuestas futbol argentino|apuestas futbol champions league|apuestas futbol chile|apuestas futbol colombia|apuestas futbol consejos|apuestas futbol en directo|apuestas fútbol en directo|apuestas futbol en vivo|apuestas fútbol en vivo|apuestas futbol españa|apuestas futbol español|apuestas fútbol español|apuestas futbol eurocopa|apuestas
futbol femenino|apuestas futbol foro|apuestas futbol gratis|apuestas futbol hoy|apuestas fútbol
hoy|apuestas futbol juegos olimpicos|apuestas futbol mexico|apuestas futbol
mundial|apuestas futbol online|apuestas futbol para hoy|apuestas futbol peru|apuestas futbol pronosticos|apuestas futbol
sala|apuestas futbol telegram|apuestas futbol virtual|apuestas galgos|apuestas
galgos en directo|apuestas galgos hoy|apuestas galgos online|apuestas galgos pronosticos|apuestas galgos trucos|apuestas gana|apuestas gana colombia|apuestas gana
resultados|apuestas ganadas|apuestas ganadas hoy|apuestas ganador champions league|apuestas ganador copa america|apuestas ganador copa del rey|apuestas ganador copa
del rey baloncesto|apuestas ganador copa libertadores|apuestas ganador
de la eurocopa|apuestas ganador de la liga|apuestas ganador del mundial|apuestas ganador eurocopa|apuestas ganador europa league|apuestas ganador f1|apuestas ganador la liga|apuestas ganador liga española|apuestas ganador mundial|apuestas ganador mundial baloncesto|apuestas ganador mundial f1|apuestas ganador nba|apuestas ganadores eurocopa|apuestas ganadores mundial|apuestas ganar champions|apuestas ganar eurocopa|apuestas
ganar liga|apuestas ganar mundial|apuestas ganar nba|apuestas getafe valencia|apuestas ghana uruguay|apuestas girona|apuestas girona athletic|apuestas girona betis|apuestas girona campeon de liga|apuestas girona campeon liga|apuestas girona
gana la liga|apuestas girona real madrid|apuestas girona real sociedad|apuestas goleador eurocopa|apuestas
goleadores eurocopa|apuestas goles asiaticos|apuestas golf|apuestas golf masters|apuestas golf pga|apuestas granada barcelona|apuestas grand slam de tenis|apuestas gratis|apuestas gratis casino|apuestas gratis con premios|apuestas gratis hoy|apuestas gratis para hoy|apuestas
gratis por registro|apuestas gratis puntos|apuestas gratis regalos|apuestas
gratis sin deposito|apuestas gratis sin depósito|apuestas gratis
sin ingreso|apuestas gratis sports|apuestas gratis y ganar premios|apuestas grupo a eurocopa|apuestas grupos eurocopa|apuestas handicap|apuestas handicap
asiatico|apuestas handicap baloncesto|apuestas handicap como funciona|apuestas handicap nba|apuestas handicap nfl|apuestas hipicas online|apuestas hípicas online|apuestas hipicas venezuela|apuestas hockey|apuestas hockey hielo|apuestas hockey patines|apuestas
hockey sobre hielo|apuestas holanda argentina|apuestas holanda vs argentina|apuestas hoy|apuestas hoy champions|apuestas hoy futbol|apuestas hoy nba|apuestas hoy pronosticos|apuestas hoy seguras|apuestas
impuestos|apuestas inglaterra paises bajos|apuestas inter barca|apuestas
inter barcelona|apuestas juego|apuestas juegos|apuestas juegos
en linea|apuestas juegos olimpicos|apuestas juegos olímpicos|apuestas juegos olimpicos baloncesto|apuestas
juegos online|apuestas juegos virtuales|apuestas jugador sevilla|apuestas jugadores
nba|apuestas kings league americas|apuestas la liga|apuestas la liga española|apuestas la liga hoy|apuestas la liga santander|apuestas las vegas
mlb|apuestas las vegas nba|apuestas las vegas nfl|apuestas league of legends mundial|apuestas
legal|apuestas legales|apuestas legales en colombia|apuestas legales en españa|apuestas
legales en estados unidos|apuestas legales españa|apuestas leganes betis|apuestas libertadores|apuestas licencia|apuestas
liga 1 peru|apuestas liga argentina|apuestas liga bbva pronosticos|apuestas liga
de campeones|apuestas liga de campeones de baloncesto|apuestas
liga de campeones de hockey|apuestas liga españa|apuestas liga española|apuestas liga santander
pronosticos|apuestas ligas de futbol|apuestas linea|apuestas linea de gol|apuestas
liverpool barcelona|apuestas liverpool real madrid|apuestas lol mundial|apuestas madrid|apuestas madrid arsenal|apuestas madrid atletico|apuestas madrid atletico champions|apuestas madrid barca|apuestas madrid barça|apuestas madrid barca hoy|apuestas
madrid barca supercopa|apuestas madrid barcelona|apuestas madrid barsa|apuestas madrid bayern|apuestas madrid
betis|apuestas madrid borussia|apuestas madrid campeon champions|apuestas madrid celta|apuestas madrid
city|apuestas madrid dortmund|apuestas madrid gana la liga|apuestas
madrid gana liga|apuestas madrid hoy|apuestas madrid liverpool|apuestas madrid osasuna|apuestas madrid sevilla|apuestas madrid valencia|apuestas madrid vs arsenal|apuestas madrid vs barcelona|apuestas mallorca osasuna|apuestas mallorca real sociedad|apuestas manchester athletic|apuestas manchester
city real madrid|apuestas mas faciles de ganar|apuestas mas seguras|apuestas mas seguras para hoy|apuestas masters de golf|apuestas masters de tenis|apuestas
maximo goleador eurocopa|apuestas maximo goleador
mundial|apuestas mejor jugador eurocopa|apuestas
mejores casinos online|apuestas mexico|apuestas méxico|apuestas mexico polonia|apuestas
méxico polonia|apuestas mlb|apuestas mlb hoy|apuestas mlb las vegas|apuestas mlb para hoy|apuestas
mlb pronosticos|apuestas mlb usa|apuestas mma ufc|apuestas momios|apuestas multiples|apuestas múltiples|apuestas multiples
como funcionan|apuestas multiples el gordo|apuestas multiples futbol|apuestas mundial|apuestas mundial 2026|apuestas mundial baloncesto|apuestas mundial
balonmano|apuestas mundial brasil|apuestas mundial campeon|apuestas mundial ciclismo|apuestas
mundial clubes|apuestas mundial de baloncesto|apuestas mundial de
ciclismo|apuestas mundial de clubes|apuestas mundial de futbol|apuestas mundial de fútbol|apuestas mundial de rugby|apuestas
mundial f1|apuestas mundial favoritos|apuestas mundial femenino|apuestas mundial formula
1|apuestas mundial futbol|apuestas mundial ganador|apuestas mundial lol|apuestas mundial moto gp|apuestas mundial motogp|apuestas mundial rugby|apuestas mundial sub 17|apuestas mundiales|apuestas mundialistas|apuestas mvp eurocopa|apuestas mvp nba|apuestas
mvp nfl|apuestas nacionales de colombia|apuestas nba|apuestas nba all
star|apuestas nba campeon|apuestas nba consejos|apuestas nba esta noche|apuestas
nba finals|apuestas nba gratis|apuestas nba hoy|apuestas nba hoy
jugadores|apuestas nba hoy pronosticos|apuestas
nba para hoy|apuestas nba playoffs|apuestas nba
pronosticos|apuestas nba pronósticos|apuestas
nba pronosticos hoy|apuestas nba tipster|apuestas nfl|apuestas nfl hoy|apuestas nfl las
vegas|apuestas nfl playoffs|apuestas nfl pronosticos|apuestas nfl pronósticos|apuestas
nfl semana 4|apuestas nfl super bowl|apuestas nhl|apuestas nhl pronosticos|apuestas
octavos eurocopa|apuestas ofertas|apuestas online|apuestas online
argentina|apuestas online argentina legal|apuestas online bono|apuestas online bono bienvenida|apuestas online
boxeo|apuestas online caballos|apuestas online carreras de caballos|apuestas online casino|apuestas online
champions league|apuestas online chile|apuestas online ciclismo|apuestas online colombia|apuestas online comparativa|apuestas online con paypal|apuestas online de caballos|apuestas online deportivas|apuestas online en argentina|apuestas online en peru|apuestas online espana|apuestas online españa|apuestas
online esports|apuestas online foro|apuestas online futbol|apuestas online futbol españa|apuestas
online golf|apuestas online gratis|apuestas online gratis sin deposito|apuestas
online juegos|apuestas online mexico|apuestas online mma|apuestas
online movil|apuestas online nba|apuestas online net|apuestas
online nuevas|apuestas online opiniones|apuestas online
paypal|apuestas online peru|apuestas online seguras|apuestas online sin dinero|apuestas
online sin registro|apuestas online tenis|apuestas online ufc|apuestas online uruguay|apuestas online venezuela|apuestas open britanico
golf|apuestas osasuna athletic|apuestas osasuna barcelona|apuestas osasuna real madrid|apuestas osasuna
sevilla|apuestas osasuna valencia|apuestas over|apuestas over 2.5|apuestas over under|apuestas paginas|apuestas pago anticipado|apuestas paises
bajos ecuador|apuestas paises bajos inglaterra|apuestas países bajos qatar|apuestas para boxeo|apuestas para champions league|apuestas para el
clasico|apuestas para el dia de hoy|apuestas para el mundial|apuestas para el partido de hoy|apuestas
para eurocopa|apuestas para europa league|apuestas para futbol|apuestas para
ganar|apuestas para ganar dinero|apuestas para ganar dinero facil|apuestas para ganar en la ruleta|apuestas para ganar la champions|apuestas para ganar la
eurocopa|apuestas para ganar la europa league|apuestas para ganar la
liga|apuestas para ganar siempre|apuestas para hacer|apuestas para hoy|apuestas para hoy de futbol|apuestas para hoy europa league|apuestas
para hoy futbol|apuestas para juegos|apuestas para la champions league|apuestas para la copa
del rey|apuestas para la eurocopa|apuestas para la europa league|apuestas para la final de la eurocopa|apuestas para la nba hoy|apuestas para
los partidos de hoy|apuestas para partidos de hoy|apuestas para ufc|apuestas partido|apuestas partido
aplazado|apuestas partido champions|apuestas partido
colombia|apuestas partido españa marruecos|apuestas partido mundial|apuestas partido suspendido|apuestas partidos|apuestas partidos champions league|apuestas partidos csgo|apuestas partidos de futbol|apuestas
partidos de futbol hoy|apuestas partidos de hoy|apuestas
partidos eurocopa|apuestas partidos futbol|apuestas partidos hoy|apuestas partidos mundial|apuestas paypal|apuestas peleas de boxeo|apuestas peru|apuestas
perú|apuestas peru brasil|apuestas peru chile|apuestas peru paraguay|apuestas peru uruguay|apuestas peru vs chile|apuestas peru vs colombia|apuestas pichichi eurocopa|apuestas plataforma|apuestas playoff|apuestas playoff ascenso|apuestas playoff ascenso a
primera|apuestas playoff nba|apuestas playoff segunda|apuestas
playoff segunda b|apuestas playoffs nba|apuestas playoffs nfl|apuestas polonia argentina|apuestas por argentina|apuestas por internet mexico|apuestas por internet para ganar dinero|apuestas
por paypal|apuestas por ronda boxeo|apuestas por sistema|apuestas portugal uruguay|apuestas pre partido|apuestas predicciones|apuestas predicciones futbol|apuestas primera division|apuestas primera division españa|apuestas promociones|apuestas pronostico|apuestas pronosticos|apuestas pronosticos deportivos|apuestas pronosticos deportivos tenis|apuestas pronosticos futbol|apuestas pronosticos gratis|apuestas pronosticos nba|apuestas pronosticos tenis|apuestas prorroga|apuestas
psg barca|apuestas psg barcelona|apuestas puntos por tarjetas|apuestas puntos tarjetas|apuestas que aceptan paypal|apuestas
que es handicap|apuestas que puedes hacer con tu novia|apuestas que siempre ganaras|apuestas que significa|apuestas quien bajara a segunda|apuestas quién bajara a segunda|apuestas quien gana el mundial|apuestas quien gana eurocopa|apuestas
quien gana la champions|apuestas quien gana la eurocopa|apuestas quien gana la liga|apuestas quien ganara el mundial|apuestas quién ganará el mundial|apuestas quien ganara la champions|apuestas quien ganara la eurocopa|apuestas quien ganara la liga|apuestas rayo barcelona|apuestas real madrid|apuestas real madrid arsenal|apuestas real madrid athletic|apuestas real madrid atletico|apuestas real madrid atletico champions|apuestas real madrid
atletico de madrid|apuestas real madrid atlético de madrid|apuestas real madrid atletico madrid|apuestas real madrid barcelona|apuestas real madrid bayern|apuestas real madrid betis|apuestas real madrid borussia|apuestas real
madrid campeon champions|apuestas real madrid celta|apuestas
real madrid champions|apuestas real madrid city|apuestas real madrid girona|apuestas real madrid hoy|apuestas real
madrid liverpool|apuestas real madrid manchester city|apuestas real madrid osasuna|apuestas
real madrid real sociedad|apuestas real madrid valencia|apuestas real madrid
villarreal|apuestas real madrid vs arsenal|apuestas real madrid vs atletico|apuestas real madrid vs atlético|apuestas real madrid vs
atletico madrid|apuestas real madrid vs barcelona|apuestas real
madrid vs betis|apuestas real madrid vs sevilla|apuestas real madrid vs valencia|apuestas real sociedad|apuestas real
sociedad athletic|apuestas real sociedad barcelona|apuestas real sociedad betis|apuestas real sociedad psg|apuestas
real sociedad real madrid|apuestas real sociedad valencia|apuestas
recomendadas hoy|apuestas regalo de bienvenida|apuestas
registro|apuestas resultado exacto|apuestas resultados|apuestas resultados eurocopa|apuestas retirada tenis|apuestas roma barcelona|apuestas roma sevilla|apuestas
rugby|apuestas rugby mundial|apuestas rugby world cup|apuestas
ruleta seguras|apuestas segunda|apuestas segunda b|apuestas segunda division|apuestas segunda división|apuestas segunda division b|apuestas segunda
division españa|apuestas seguras|apuestas seguras baloncesto|apuestas seguras calculadora|apuestas seguras en la ruleta|apuestas seguras eurocopa|apuestas seguras
foro|apuestas seguras futbol|apuestas seguras futbol hoy|apuestas seguras gratis|apuestas seguras hoy|apuestas seguras hoy futbol|apuestas seguras nba|apuestas
seguras nba hoy|apuestas seguras para este fin de semana|apuestas seguras para ganar dinero|apuestas seguras para hoy|apuestas seguras para hoy fútbol|apuestas seguras para hoy pronósticos|apuestas seguras para mañana|apuestas seguras ruleta|apuestas seguras telegram|apuestas seguras tenis|apuestas semifinales
eurocopa|apuestas senegal paises bajos|apuestas
sevilla|apuestas sevilla athletic|apuestas sevilla atletico de madrid|apuestas sevilla barcelona|apuestas sevilla betis|apuestas
sevilla campeon liga|apuestas sevilla celta|apuestas sevilla gana la liga|apuestas sevilla girona|apuestas sevilla inter|apuestas sevilla jugador|apuestas sevilla juventus|apuestas sevilla leganes|apuestas sevilla madrid|apuestas sevilla
manchester united|apuestas sevilla osasuna|apuestas sevilla real madrid|apuestas sevilla real sociedad|apuestas sevilla roma|apuestas sevilla valencia|apuestas significa|apuestas
simples ejemplos|apuestas simples o combinadas|apuestas sin deposito|apuestas sin deposito inicial|apuestas sin deposito minimo|apuestas sin dinero|apuestas
sin dinero real|apuestas sin empate|apuestas sin empate
que significa|apuestas sin ingreso minimo|apuestas sin registro|apuestas sistema|apuestas sistema calculadora|apuestas
sistema como funciona|apuestas sistema trixie|apuestas sociedad|apuestas
sorteo copa del rey|apuestas stake|apuestas stake 10|apuestas stake 10 hoy|apuestas super bowl favorito|apuestas super rugby|apuestas supercopa españa|apuestas superliga argentina|apuestas tarjeta roja|apuestas tarjetas|apuestas tarjetas amarillas|apuestas tenis|apuestas tenis atp|apuestas tenis consejos|apuestas tenis copa davis|apuestas tenis de mesa|apuestas
tenis de mesa pronosticos|apuestas tenis en vivo|apuestas tenis femenino|apuestas tenis
hoy|apuestas tenis itf|apuestas tenis pronosticos|apuestas tenis pronósticos|apuestas tenis retirada|apuestas tenis
roland garros|apuestas tenis seguras|apuestas tenis wimbledon|apuestas
tenis wta|apuestas tercera division|apuestas tercera division españa|apuestas tipos|apuestas
tips|apuestas tipster|apuestas tipster para hoy|apuestas topuria holloway cuotas|apuestas torneos de golf|apuestas torneos de tenis|apuestas trucos|apuestas uefa champions league|apuestas uefa europa
league|apuestas ufc|apuestas ufc chile|apuestas ufc como funciona|apuestas ufc hoy|apuestas ufc ilia topuria|apuestas ufc online|apuestas ufc pronósticos|apuestas ufc telegram|apuestas ufc topuria|apuestas under over|apuestas unionistas
villarreal|apuestas uruguay|apuestas uruguay colombia|apuestas uruguay corea|apuestas uruguay vs colombia|apuestas us open golf|apuestas us open tenis|apuestas valencia|apuestas valencia barcelona|apuestas valencia betis|apuestas valencia madrid|apuestas valencia real madrid|apuestas valladolid barcelona|apuestas valladolid valencia|apuestas valor
app|apuestas valor en directo|apuestas valor galgos|apuestas venezuela|apuestas venezuela argentina|apuestas venezuela bolivia|apuestas venezuela ecuador|apuestas villarreal|apuestas villarreal athletic|apuestas villarreal barcelona|apuestas villarreal
bayern|apuestas villarreal betis|apuestas villarreal liverpool|apuestas villarreal manchester|apuestas villarreal manchester united|apuestas villarreal vs real madrid|apuestas virtuales|apuestas virtuales colombia|apuestas virtuales futbol|apuestas virtuales sin dinero|apuestas vivo|apuestas vuelta a
españa|apuestas vuelta españa|apuestas william hill partidos de
hoy|apuestas y casino|apuestas y casinos|apuestas y juegos de azar|apuestas y pronosticos|apuestas y pronosticos de futbol|apuestas y pronosticos deportivos|apuestas y resultados|apuestas-deportivas|apuestas-deportivas.es pronosticos|arbitro nba apuestas|argentina apuestas|argentina colombia apuestas|argentina croacia
apuestas|argentina francia apuestas|argentina mexico apuestas|argentina peru
apuestas|argentina uruguay apuestas|argentina vs bolivia apuestas|argentina vs chile apuestas|argentina
vs colombia apuestas|argentina vs francia apuestas|argentina vs.
colombia apuestas|asi se gana en las apuestas deportivas|asiatico apuestas|asiatico en apuestas|asiaticos apuestas|athletic barcelona apuestas|athletic manchester united apuestas|athletic osasuna apuestas|athletic real madrid apuestas|atletico
barcelona apuestas|atletico de madrid apuestas|atlético de madrid
apuestas|atletico de madrid real madrid apuestas|atletico de madrid vs barcelona apuestas|atletico madrid
real madrid apuestas|atletico madrid vs real madrid apuestas|atletico real madrid apuestas|atletico
vs real madrid apuestas|avisador de cuotas apuestas|bajada de cuotas apuestas|baloncesto apuestas|barbastro
barcelona apuestas|barca apuestas|barca bayern apuestas|barca
inter apuestas|barca madrid apuestas|barça madrid apuestas|barca vs atletico
apuestas|barca vs madrid apuestas|barca vs real madrid apuestas|barcelona – real madrid apuestas|barcelona apuestas|barcelona atletico apuestas|barcelona atletico de madrid apuestas|barcelona atletico
madrid apuestas|barcelona betis apuestas|barcelona casa de apuestas|barcelona inter apuestas|barcelona psg apuestas|barcelona real madrid apuestas|barcelona real sociedad apuestas|barcelona sevilla apuestas|barcelona valencia
apuestas|barcelona vs athletic bilbao apuestas|barcelona vs atlético madrid apuestas|barcelona vs
betis apuestas|barcelona vs celta de vigo apuestas|barcelona vs espanyol apuestas|barcelona vs girona apuestas|barcelona vs madrid apuestas|barcelona vs real madrid apuestas|barcelona vs real sociedad apuestas|barcelona vs sevilla
apuestas|barcelona vs villarreal apuestas|base de datos cuotas apuestas deportivas|bayern real madrid apuestas|beisbol apuestas|best america apuestas|bet apuestas chile|bet apuestas
en vivo|betis – chelsea apuestas|betis apuestas|betis barcelona apuestas|betis chelsea apuestas|betis madrid apuestas|betis sevilla
apuestas|betsson tu sitio de apuestas online|blog apuestas baloncesto|blog apuestas ciclismo|blog apuestas nba|blog apuestas
tenis|blog de apuestas de tenis|bono apuestas|bono apuestas deportivas|bono apuestas deportivas sin deposito|bono apuestas gratis|bono apuestas gratis
sin deposito|bono apuestas sin deposito|bono bienvenida apuestas|bono
bienvenida apuestas deportivas|bono bienvenida apuestas españa|bono bienvenida apuestas sin deposito|bono bienvenida apuestas sin depósito|bono
bienvenida casa apuestas|bono bienvenida casa de apuestas|bono bienvenida marca apuestas|bono casa apuestas|bono casa de apuestas|bono casa
de apuestas sin ingreso|bono casas de apuestas|bono de apuestas|bono de apuestas gratis sin deposito|bono de bienvenida apuestas|bono de bienvenida apuestas deportivas|bono de
bienvenida casa de apuestas|bono de bienvenida casas de apuestas|bono de casas de apuestas|bono de registro apuestas|bono de registro
apuestas deportivas|bono de registro casa de apuestas|bono
gratis apuestas|bono marca apuestas|bono por registro apuestas|bono por registro apuestas deportivas|bono por registro casa de apuestas|bono registro
apuestas|bono sin deposito apuestas|bono sin depósito apuestas|bono sin deposito
apuestas deportivas|bono sin depósito apuestas deportivas|bono sin deposito casa de apuestas|bono
sin deposito marca apuestas|bono sin ingreso apuestas|bono sin ingreso apuestas deportivas|bonos apuestas|bonos
apuestas colombia|bonos apuestas deportivas|bonos apuestas deportivas sin deposito|bonos apuestas gratis|bonos apuestas
sin deposito|bonos apuestas sin depósito|bonos
bienvenida apuestas|bonos bienvenida casas apuestas|bonos
bienvenida casas de apuestas|bonos casa de apuestas|bonos casas apuestas|bonos casas de apuestas|bonos casas de apuestas
colombia|bonos casas de apuestas deportivas|bonos casas de apuestas españa|bonos casas
de apuestas nuevas|bonos casas de apuestas sin deposito|bonos casas de apuestas sin depósito|bonos de apuestas|bonos
de apuestas deportivas|bonos de apuestas gratis|bonos de apuestas sin deposito|bonos de bienvenida
apuestas|bonos de bienvenida apuestas deportivas|bonos de bienvenida casa
de apuestas|bonos de bienvenida casas de apuestas|bonos de bienvenida de
casas de apuestas|bonos de bienvenida en casas de apuestas|bonos de casas de apuestas|bonos de
casas de apuestas sin deposito|bonos en casa de apuestas|bonos en casas de apuestas sin deposito|bonos gratis apuestas|bonos gratis apuestas deportivas|bonos gratis casas de
apuestas|bonos gratis sin deposito apuestas|bonos paginas de apuestas|bonos
registro casas de apuestas|bonos sin deposito apuestas|bonos sin depósito
apuestas|bonos sin deposito apuestas deportivas|bonos sin deposito
casas de apuestas|bot de apuestas deportivas gratis|boxeo apuestas|brasil colombia
apuestas|brasil peru apuestas|brasil vs colombia apuestas|buenas apuestas para hoy|buscador cuotas apuestas|buscador de apuestas seguras|buscador de cuotas
apuestas|buscador de cuotas de apuestas|buscar
apuestas seguras|caballos apuestas|calculador de apuestas|calculador
de cuotas apuestas|calculadora apuestas|calculadora apuestas combinadas|calculadora apuestas
de sistema|calculadora apuestas deportivas|calculadora apuestas deportivas seguras|calculadora apuestas multiples|calculadora apuestas segura|calculadora apuestas seguras|calculadora apuestas
sistema|calculadora apuestas yankee|calculadora arbitraje apuestas|calculadora cubrir apuestas|calculadora cuotas apuestas|calculadora de apuestas|calculadora de apuestas combinadas|calculadora de apuestas de futbol|calculadora de apuestas de sistema|calculadora de apuestas deportivas|calculadora
de apuestas multiples|calculadora de apuestas seguras|calculadora de apuestas sistema|calculadora de apuestas surebets|calculadora
de arbitraje apuestas|calculadora de cuotas apuestas|calculadora de
cuotas de apuestas|calculadora para apuestas deportivas|calculadora
poisson apuestas|calculadora poisson apuestas deportivas|calculadora poisson para apuestas|calculadora scalping apuestas deportivas|calculadora sistema apuestas|calculadora stake apuestas|calculadora trading apuestas|calcular apuestas|calcular apuestas deportivas|calcular apuestas futbol|calcular apuestas sistema|calcular cuotas apuestas|calcular cuotas apuestas
combinadas|calcular cuotas apuestas deportivas|calcular cuotas de apuestas|calcular ganancias
apuestas deportivas|calcular momios apuestas|calcular probabilidad cuota apuestas|calcular stake apuestas|calcular unidades apuestas|calcular
yield apuestas|calculo de apuestas|calculo de apuestas deportivas|cambio de cuotas apuestas|campeon champions apuestas|campeon eurocopa apuestas|campeon liga apuestas|campeon nba
apuestas|canales de apuestas gratis|carrera de caballos apuestas|carrera de caballos apuestas
juego|carrera de caballos con apuestas|carrera de galgos apuestas|carreras de
caballos apuestas|carreras de caballos apuestas online|carreras de caballos con apuestas|carreras de caballos
juegos de apuestas|carreras de galgos apuestas|carreras de galgos apuestas online|carreras
de galgos apuestas trucos|carreras galgos apuestas|casa apuestas argentina|casa
apuestas atletico de madrid|casa apuestas barcelona|casa apuestas betis|casa apuestas
bono bienvenida|casa apuestas bono gratis|casa apuestas bono sin deposito|casa apuestas cerca
de mi|casa apuestas chile|casa apuestas colombia|casa
apuestas con mejores cuotas|casa apuestas deportivas|casa apuestas españa|casa apuestas española|casa apuestas eurocopa|casa apuestas futbol|casa apuestas mejores cuotas|casa
apuestas mundial|casa apuestas nueva|casa apuestas nuevas|casa
apuestas online|casa apuestas peru|casa apuestas valencia|casa de apuestas|casa de apuestas 10 euros gratis|casa
de apuestas argentina|casa de apuestas atletico
de madrid|casa de apuestas baloncesto|casa de apuestas barcelona|casa de apuestas beisbol|casa
de apuestas betis|casa de apuestas bono|casa de apuestas
bono bienvenida|casa de apuestas bono de bienvenida|casa de apuestas bono gratis|casa
de apuestas bono por registro|casa de apuestas bono sin deposito|casa de apuestas boxeo|casa de apuestas caballos|casa de apuestas carreras de caballos|casa de apuestas cerca
de mi|casa de apuestas cerca de mí|casa de apuestas champions
league|casa de apuestas chile|casa de apuestas ciclismo|casa de apuestas colombia|casa de apuestas con bono de bienvenida|casa de apuestas con bono sin deposito|casa de apuestas con cuotas mas altas|casa
de apuestas con esports|casa de apuestas con las mejores cuotas|casa de apuestas con licencia en españa|casa de apuestas
con mejores cuotas|casa de apuestas con pago anticipado|casa de apuestas con paypal|casa de apuestas copa america|casa de apuestas
de caballos|casa de apuestas de colombia|casa de apuestas de españa|casa de apuestas de futbol|casa de apuestas de fútbol|casa de apuestas de futbol peru|casa de
apuestas de peru|casa de apuestas del madrid|casa de apuestas del real madrid|casa de apuestas
deportivas|casa de apuestas deportivas cerca de mi|casa de apuestas deportivas en argentina|casa de apuestas deportivas en chile|casa de apuestas deportivas
en colombia|casa de apuestas deportivas en españa|casa de apuestas deportivas en madrid|casa de apuestas deportivas
españa|casa de apuestas deportivas españolas|casa de apuestas deportivas madrid|casa de apuestas deportivas mexico|casa de apuestas deportivas
online|casa de apuestas deportivas peru|casa de apuestas deposito 5 euros|casa de apuestas deposito minimo|casa de apuestas deposito minimo 1 euro|casa de apuestas depósito mínimo 1 euro|casa de apuestas en españa|casa de apuestas en linea|casa de apuestas
en madrid|casa de apuestas en perú|casa de apuestas
en vivo|casa de apuestas españa|casa de apuestas españa inglaterra|casa de apuestas española|casa de
apuestas españolas|casa de apuestas esports|casa de apuestas eurocopa|casa de
apuestas europa league|casa de apuestas f1|casa de apuestas formula
1|casa de apuestas futbol|casa de apuestas ingreso minimo|casa de apuestas ingreso minimo 1 euro|casa de
apuestas ingreso mínimo 1 euro|casa de apuestas legales|casa de apuestas legales en colombia|casa de apuestas legales en españa|casa de apuestas libertadores|casa de apuestas liga
española|casa de apuestas madrid|casa de apuestas mas segura|casa de apuestas mejores|casa de apuestas méxico|casa de apuestas minimo 5 euros|casa de apuestas mlb|casa de apuestas mundial|casa de apuestas
nba|casa de apuestas nfl|casa de apuestas nueva|casa de apuestas nuevas|casa de apuestas oficial del real madrid|casa
de apuestas oficial real madrid|casa de apuestas
online|casa de apuestas online argentina|casa
de apuestas online chile|casa de apuestas online españa|casa de apuestas online mexico|casa de
apuestas online paraguay|casa de apuestas online peru|casa de apuestas online usa|casa de apuestas online venezuela|casa de apuestas pago anticipado|casa de apuestas para boxeo|casa
de apuestas para ufc|casa de apuestas peru|casa de
apuestas perú|casa de apuestas peru online|casa
de apuestas por paypal|casa de apuestas promociones|casa de apuestas que regalan dinero|casa de apuestas real madrid|casa de apuestas
regalo de bienvenida|casa de apuestas sevilla|casa de apuestas sin dinero|casa de apuestas
sin ingreso minimo|casa de apuestas sin licencia en españa|casa de apuestas
sin minimo de ingreso|casa de apuestas stake|casa de apuestas tenis|casa de apuestas ufc|casa de apuestas valencia|casa de apuestas venezuela|casa de apuestas virtuales|casa de apuestas vive la
suerte|casa oficial de apuestas del real madrid|casas apuestas
asiaticas|casas apuestas bono sin deposito|casas apuestas bonos sin deposito|casas apuestas caballos|casas apuestas
chile|casas apuestas ciclismo|casas apuestas con licencia|casas apuestas con licencia en españa|casas
apuestas deportivas|casas apuestas deportivas colombia|casas apuestas deportivas
españa|casas apuestas deportivas españolas|casas apuestas deportivas nuevas|casas apuestas españa|casas
apuestas españolas|casas apuestas esports|casas apuestas eurocopa|casas apuestas golf|casas apuestas ingreso minimo
5 euros|casas apuestas legales|casas apuestas legales
españa|casas apuestas licencia|casas apuestas licencia españa|casas apuestas mexico|casas
apuestas mundial|casas apuestas nba|casas apuestas nuevas|casas apuestas nuevas españa|casas apuestas ofertas|casas apuestas online|casas apuestas paypal|casas apuestas peru|casas apuestas sin licencia|casas apuestas tenis|casas asiaticas
apuestas|casas de apuestas|casas de apuestas 5 euros|casas de apuestas app|casas de
apuestas argentinas|casas de apuestas asiaticas|casas de apuestas baloncesto|casas
de apuestas barcelona|casas de apuestas bono bienvenida|casas de apuestas bono de bienvenida|casas de apuestas bono por registro|casas de apuestas bono sin deposito|casas de apuestas bono sin ingreso|casas de apuestas bonos|casas de apuestas bonos de bienvenida|casas de apuestas bonos
gratis|casas de apuestas bonos sin deposito|casas de apuestas boxeo|casas de apuestas caballos|casas de apuestas carreras de caballos|casas de apuestas casino|casas de
apuestas casino online|casas de apuestas cerca de mi|casas
de apuestas champions league|casas de apuestas chile|casas de apuestas ciclismo|casas de
apuestas colombia|casas de apuestas com|casas
de apuestas con app|casas de apuestas con apuestas gratis|casas de apuestas con bono|casas de
apuestas con bono de bienvenida|casas de apuestas con bono de registro|casas de apuestas con bono por registro|casas de apuestas con bono sin deposito|casas de apuestas con bonos|casas de apuestas con bonos gratis|casas
de apuestas con bonos sin deposito|casas de apuestas con deposito minimo|casas de apuestas con esports|casas
de apuestas con handicap asiatico|casas de apuestas con licencia|casas de apuestas
con licencia en españa|casas de apuestas con licencia españa|casas de apuestas con licencia española|casas de apuestas con mejores cuotas|casas
de apuestas con pago anticipado|casas de apuestas con paypal|casas de apuestas con paypal en perú|casas de apuestas con promociones|casas
de apuestas con ruleta en vivo|casas de apuestas copa del rey|casas de apuestas de caballos|casas de apuestas de españa|casas
de apuestas de futbol|casas de apuestas de fútbol|casas de apuestas
de peru|casas de apuestas deportivas|casas de apuestas deportivas asiaticas|casas de
apuestas deportivas colombia|casas de apuestas deportivas comparativa|casas
de apuestas deportivas con paypal|casas de
apuestas deportivas en chile|casas de apuestas deportivas en españa|casas de apuestas deportivas en linea|casas de apuestas deportivas en madrid|casas de apuestas deportivas
en mexico|casas de apuestas deportivas en peru|casas de apuestas deportivas en sevilla|casas de apuestas deportivas en valencia|casas de apuestas deportivas españa|casas de apuestas deportivas españolas|casas de apuestas deportivas legales|casas de
apuestas deportivas madrid|casas de apuestas deportivas mexico|casas de apuestas deportivas nuevas|casas de apuestas deportivas online|casas
de apuestas deportivas peru|casas de apuestas deportivas perú|casas de apuestas deposito minimo 1 euro|casas de apuestas depósito mínimo 1 euro|casas
de apuestas dinero gratis|casas de apuestas en argentina|casas de apuestas en barcelona|casas de apuestas en chile|casas
de apuestas en colombia|casas de apuestas en españa|casas de apuestas en españa online|casas de apuestas en linea|casas de apuestas en madrid|casas de apuestas en méxico|casas de apuestas en peru|casas de apuestas en perú|casas
de apuestas en sevilla|casas de apuestas en uruguay|casas de apuestas en valencia|casas
de apuestas en venezuela|casas de apuestas equipos de
futbol|casas de apuestas españa|casas de apuestas españa alemania|casas de apuestas españa inglaterra|casas de apuestas españa licencia|casas de apuestas españa nuevas|casas de apuestas españa online|casas de apuestas
española|casas de apuestas españolas|casas de apuestas españolas
con licencia|casas de apuestas españolas online|casas de apuestas
esports|casas de apuestas eurocopa|casas de apuestas eurocopa 2024|casas de apuestas europa league|casas
de apuestas f1|casas de apuestas fisicas en barcelona|casas de apuestas fisicas en españa|casas de
apuestas formula 1|casas de apuestas fuera de españa|casas de
apuestas futbol|casas de apuestas fútbol|casas de apuestas futbol españa|casas de apuestas ganador
eurocopa|casas de apuestas gratis|casas
de apuestas ingreso minimo|casas de apuestas ingreso
minimo 1 euro|casas de apuestas ingreso minimo 5 euros|casas de apuestas inter barcelona|casas de apuestas legales|casas de apuestas legales
en colombia|casas de apuestas legales en españa|casas de apuestas
legales en mexico|casas de apuestas legales españa|casas
de apuestas legales mx|casas de apuestas licencia|casas de apuestas licencia
españa|casas de apuestas lista|casas de apuestas
madrid|casas de apuestas mas seguras|casas de apuestas mejores bonos|casas
de apuestas mejores cuotas|casas de apuestas mexico|casas de apuestas méxico|casas de apuestas minimo 5 euros|casas de apuestas
mlb|casas de apuestas mundial|casas de apuestas mundial baloncesto|casas de apuestas mundiales|casas de apuestas nba|casas de apuestas no reguladas en españa|casas de apuestas nueva ley|casas de apuestas nuevas|casas
de apuestas nuevas en colombia|casas de apuestas nuevas en españa|casas de
apuestas nuevas españa|casas de apuestas ofertas|casas de apuestas online|casas de
apuestas online argentina|casas de apuestas online colombia|casas de apuestas online deportivas|casas de apuestas online ecuador|casas de apuestas online en argentina|casas de apuestas online en chile|casas de
apuestas online en colombia|casas de apuestas online en españa|casas
de apuestas online en mexico|casas de apuestas online españa|casas de apuestas
online mas fiables|casas de apuestas online mexico|casas de apuestas online nuevas|casas de apuestas
online peru|casas de apuestas online usa|casas de apuestas online venezuela|casas de
apuestas pago paypal|casas de apuestas para ufc|casas de apuestas
paypal|casas de apuestas peru bono sin deposito|casas de apuestas presenciales en españa|casas
(10 euros gratis apuestas|10 mejores casas de
apuestas|10 trucos para ganar apuestas|15 euros gratis marca apuestas|1×2 apuestas|1×2 apuestas deportivas|1×2 apuestas que significa|1×2 en apuestas|1×2 en apuestas que significa|1×2 que significa en apuestas|5
euros gratis apuestas|9 apuestas que siempre ganaras|a partir de cuanto se declara apuestas|actividades de juegos de azar y apuestas|ad apuestas deportivas|aleksandre topuria ufc apuestas|algoritmo para
ganar apuestas deportivas|america apuestas|análisis nba
apuestas|aplicacion android apuestas deportivas|aplicacion apuestas
deportivas|aplicacion apuestas deportivas android|aplicación de apuestas online|aplicacion para hacer apuestas|aplicacion para hacer apuestas de futbol|aplicación para hacer apuestas de fútbol|aplicaciones apuestas deportivas android|aplicaciones apuestas deportivas gratis|aplicaciones de apuestas android|aplicaciones
de apuestas de fútbol|aplicaciones de apuestas deportivas|aplicaciones de apuestas deportivas peru|aplicaciones de apuestas deportivas perú|aplicaciones de apuestas en colombia|aplicaciones
de apuestas gratis|aplicaciones de apuestas online|aplicaciones de apuestas seguras|aplicaciones de
apuestas sin dinero|aplicaciones para hacer apuestas|apostar seguro apuestas deportivas|app
android apuestas deportivas|app apuestas|app apuestas android|app apuestas de futbol|app apuestas deportivas|app apuestas deportivas android|app apuestas deportivas argentina|app apuestas deportivas colombia|app
apuestas deportivas ecuador|app apuestas deportivas españa|app
apuestas deportivas gratis|app apuestas entre amigos|app apuestas futbol|app apuestas gratis|app apuestas sin dinero|app casa de
apuestas|app casas de apuestas|app control apuestas|app de apuestas|app de apuestas android|app de apuestas casino|app
de apuestas colombia|app de apuestas con bono de bienvenida|app
de apuestas de futbol|app de apuestas deportivas|app de apuestas deportivas android|app de apuestas deportivas argentina|app de
apuestas deportivas colombia|app de apuestas
deportivas en españa|app de apuestas deportivas peru|app de
apuestas deportivas perú|app de apuestas deportivas sin dinero|app de apuestas ecuador|app de apuestas en colombia|app de apuestas
en españa|app de apuestas en venezuela|app de apuestas futbol|app de apuestas gratis|app de apuestas online|app de apuestas para android|app de apuestas para ganar dinero|app de apuestas peru|app de apuestas reales|app de casas
de apuestas|app marca apuestas android|app moviles
de apuestas|app para apuestas|app para apuestas de futbol|app para apuestas deportivas|app para apuestas deportivas en español|app
para ganar apuestas deportivas|app para hacer apuestas|app para hacer apuestas deportivas|app para hacer apuestas entre amigos|app
para llevar control de apuestas|app pronosticos apuestas deportivas|app versus apuestas|apps apuestas mundial|apps
de apuestas|apps de apuestas con bono de
bienvenida|apps de apuestas de futbol|apps de apuestas deportivas peru|apps de apuestas mexico|apps
para apuestas|aprender a hacer apuestas deportivas|aprender
hacer apuestas deportivas|apuesta del dia apuestas deportivas|apuestas 10 euros
gratis|apuestas 100 seguras|apuestas 1×2|apuestas 1X2|apuestas
2 division|apuestas 3 division|apuestas a caballos|apuestas a carreras de caballos|apuestas a colombia|apuestas a corners|apuestas a ganar|apuestas a jugadores nba|apuestas a la baja|apuestas a
la nfl|apuestas al barcelona|apuestas al dia|apuestas
al empate|apuestas al mundial|apuestas al tenis wta|apuestas alaves barcelona|apuestas alcaraz hoy|apuestas alemania españa|apuestas
alonso campeon del mundo|apuestas altas y bajas|apuestas altas y bajas nfl|apuestas ambos equipos marcan|apuestas america|apuestas android|apuestas anillo nba|apuestas antes del mundial|apuestas anticipadas|apuestas anticipadas nba|apuestas apps|apuestas arabia
argentina|apuestas argentina|apuestas argentina campeon del mundo|apuestas argentina canada|apuestas argentina
colombia|apuestas argentina croacia|apuestas argentina españa|apuestas argentina francia|apuestas argentina francia cuanto paga|apuestas argentina francia mundial|apuestas argentina gana el mundial|apuestas argentina gana mundial|apuestas argentina holanda|apuestas argentina mexico|apuestas
argentina méxico|apuestas argentina mundial|apuestas argentina
online|apuestas argentina paises bajos|apuestas argentina polonia|apuestas argentina uruguay|apuestas argentina vs australia|apuestas argentina vs colombia|apuestas argentina
vs francia|apuestas argentina vs peru|apuestas argentinas|apuestas
arsenal real madrid|apuestas ascenso a primera division|apuestas ascenso a segunda|apuestas asiaticas|apuestas asiatico|apuestas athletic|apuestas athletic atletico|apuestas athletic barça|apuestas athletic barcelona|apuestas athletic betis|apuestas athletic manchester|apuestas athletic manchester united|apuestas athletic osasuna|apuestas athletic real|apuestas athletic real
madrid|apuestas athletic real sociedad|apuestas athletic real sociedad
final|apuestas athletic roma|apuestas athletic sevilla|apuestas athletic valencia|apuestas atletico|apuestas atletico barcelona|apuestas atletico barsa|apuestas atletico campeon champions|apuestas
atletico campeon de liga|apuestas atlético copenhague|apuestas atletico de madrid|apuestas atlético de madrid|apuestas atletico de madrid barcelona|apuestas atletico de madrid
gana la liga|apuestas atletico de madrid real madrid|apuestas atlético
de madrid real madrid|apuestas atletico de madrid vs barcelona|apuestas atletico madrid|apuestas atletico madrid real madrid|apuestas atletico madrid vs barcelona|apuestas atletico real madrid|apuestas atletico real madrid champions|apuestas atletismo|apuestas bajas|apuestas baloncesto|apuestas baloncesto acb|apuestas baloncesto handicap|apuestas baloncesto hoy|apuestas baloncesto
juegos olimpicos|apuestas baloncesto nba|apuestas baloncesto pronostico|apuestas baloncesto pronósticos|apuestas baloncesto prorroga|apuestas barca|apuestas barca athletic|apuestas barca atletico|apuestas
barca bayern|apuestas barca bayern munich|apuestas barca girona|apuestas barca hoy|apuestas barça hoy|apuestas barca inter|apuestas
barca juventus|apuestas barca madrid|apuestas barça madrid|apuestas barca real madrid|apuestas barca vs juve|apuestas barca vs madrid|apuestas barca vs psg|apuestas barcelona|apuestas barcelona alaves|apuestas barcelona athletic|apuestas barcelona atletico|apuestas barcelona atletico de madrid|apuestas
barcelona atlético de madrid|apuestas barcelona atletico madrid|apuestas barcelona bayern|apuestas barcelona
betis|apuestas barcelona campeon de liga|apuestas barcelona
celta|apuestas barcelona espanyol|apuestas barcelona gana
la champions|apuestas barcelona girona|apuestas barcelona granada|apuestas barcelona hoy|apuestas barcelona inter|apuestas barcelona madrid|apuestas barcelona osasuna|apuestas barcelona psg|apuestas barcelona real madrid|apuestas barcelona real sociedad|apuestas barcelona sevilla|apuestas barcelona valencia|apuestas barcelona
villarreal|apuestas barcelona vs atletico madrid|apuestas
barcelona vs madrid|apuestas barcelona vs real madrid|apuestas barsa
madrid|apuestas basket hoy|apuestas bayern barcelona|apuestas bayern vs barcelona|apuestas beisbol|apuestas béisbol|apuestas
beisbol mlb|apuestas beisbol pronosticos|apuestas beisbol venezolano|apuestas betis|apuestas betis
– chelsea|apuestas betis barcelona|apuestas betis chelsea|apuestas betis fiorentina|apuestas betis girona|apuestas betis madrid|apuestas betis mallorca|apuestas betis real madrid|apuestas betis real sociedad|apuestas
betis sevilla|apuestas betis valencia|apuestas betis valladolid|apuestas betis vs
valencia|apuestas betplay hoy colombia|apuestas betsson peru|apuestas bienvenida|apuestas billar
online|apuestas bolivia vs colombia|apuestas bono|apuestas bono bienvenida|apuestas bono de bienvenida|apuestas bono de bienvenida sin deposito|apuestas bono gratis|apuestas
bono sin deposito|apuestas bonos sin deposito|apuestas
borussia real madrid|apuestas boxeo|apuestas boxeo de campeonato|apuestas boxeo
españa|apuestas boxeo español|apuestas boxeo femenino olimpiadas|apuestas boxeo
hoy|apuestas boxeo online|apuestas brasil colombia|apuestas brasil
peru|apuestas brasil uruguay|apuestas brasil vs colombia|apuestas brasil vs peru|apuestas caballos|apuestas caballos colocado|apuestas caballos españa|apuestas caballos hipodromo|apuestas caballos
hoy|apuestas caballos madrid|apuestas caballos online|apuestas caballos sanlucar de barrameda|apuestas
caballos zarzuela|apuestas calculador|apuestas campeon|apuestas campeon champions|apuestas campeón champions|apuestas campeon champions 2025|apuestas campeon champions league|apuestas
campeon conference league|apuestas campeon copa
america|apuestas campeon copa del rey|apuestas campeon de champions|apuestas
campeon de la champions|apuestas campeon de liga|apuestas campeon del mundo|apuestas campeon eurocopa|apuestas campeón eurocopa|apuestas campeon europa league|apuestas campeon f1|apuestas campeon f1 2025|apuestas campeon formula 1|apuestas campeon libertadores|apuestas campeon liga|apuestas campeon liga bbva|apuestas campeon liga
española|apuestas campeon liga santander|apuestas campeon motogp 2025|apuestas campeon mundial|apuestas campeón mundial|apuestas campeon mundial baloncesto|apuestas
campeon nba|apuestas campeón nba|apuestas campeon premier|apuestas campeon premier
league|apuestas campeon roland garros|apuestas campeonato f1|apuestas campeonatos
de futbol|apuestas carrera de caballos|apuestas carrera de caballos
hoy|apuestas carrera de caballos nocturnas|apuestas carrera de galgos fin de semana|apuestas carrera de galgos hoy|apuestas carrera de galgos nocturnas|apuestas carreras caballos|apuestas carreras caballos
sanlucar|apuestas carreras de caballos|apuestas carreras de caballos en directo|apuestas carreras de
caballos en vivo|apuestas carreras de caballos españa|apuestas carreras de caballos hoy|apuestas carreras de
caballos nacionales|apuestas carreras de caballos nocturnas|apuestas carreras de caballos online|apuestas carreras de caballos sanlucar|apuestas carreras de
caballos sanlúcar|apuestas carreras de galgos|apuestas carreras de galgos en vivo|apuestas carreras de galgos nocturnas|apuestas carreras de galgos pre partido|apuestas casino|apuestas casino barcelona|apuestas casino futbol|apuestas casino gran madrid|apuestas
casino gratis|apuestas casino madrid|apuestas casino online|apuestas casino online argentina|apuestas casinos|apuestas casinos online|apuestas celta|apuestas celta barcelona|apuestas celta betis|apuestas celta eibar|apuestas celta espanyol|apuestas celta granada|apuestas celta madrid|apuestas celta manchester|apuestas celta
real madrid|apuestas champion league|apuestas champions foro|apuestas champions
hoy|apuestas champions league|apuestas champions
league – pronósticos|apuestas champions league 2025|apuestas champions league hoy|apuestas champions league pronosticos|apuestas champions league pronósticos|apuestas champions pronosticos|apuestas chelsea barcelona|apuestas chelsea betis|apuestas
chile|apuestas chile peru|apuestas chile venezuela|apuestas chile vs colombia|apuestas chile vs uruguay|apuestas ciclismo|apuestas ciclismo en vivo|apuestas ciclismo femenino|apuestas ciclismo
tour francia|apuestas ciclismo vuelta|apuestas ciclismo vuelta
a españa|apuestas ciclismo vuelta españa|apuestas
city madrid|apuestas city real madrid|apuestas clasico|apuestas clasico español|apuestas clasico real madrid barcelona|apuestas
clasificacion mundial|apuestas colombia|apuestas colombia argentina|apuestas colombia brasil|apuestas
colombia paraguay|apuestas colombia uruguay|apuestas colombia vs argentina|apuestas
colombia vs brasil|apuestas combinadas|apuestas combinadas
como funcionan|apuestas combinadas de futbol|apuestas combinadas
de fútbol|apuestas combinadas foro|apuestas combinadas futbol|apuestas combinadas hoy|apuestas
combinadas mismo partido|apuestas combinadas mundial|apuestas
combinadas nba|apuestas combinadas para esta semana|apuestas combinadas para hoy|apuestas combinadas para mañana|apuestas combinadas pronosticos|apuestas combinadas recomendadas|apuestas combinadas seguras|apuestas
combinadas seguras para hoy|apuestas combinadas seguras para
mañana|apuestas como ganar|apuestas comparador|apuestas
con bono de bienvenida|apuestas con dinero ficticio|apuestas con dinero real|apuestas con dinero virtual|apuestas con handicap|apuestas con handicap asiatico|apuestas con handicap baloncesto|apuestas con mas probabilidades de ganar|apuestas con paypal|apuestas con tarjeta de credito|apuestas con tarjeta
de debito|apuestas consejos|apuestas copa|apuestas copa africa|apuestas copa america|apuestas copa américa|apuestas copa argentina|apuestas copa brasil|apuestas copa davis|apuestas copa de europa|apuestas copa del mundo|apuestas copa del rey|apuestas copa del rey baloncesto|apuestas copa del rey final|apuestas copa
del rey futbol|apuestas copa del rey ganador|apuestas copa del rey hoy|apuestas copa del rey pronosticos|apuestas copa del rey
pronósticos|apuestas copa europa|apuestas copa italia|apuestas copa libertadores|apuestas copa
mundial de hockey|apuestas copa rey|apuestas copa sudamericana|apuestas corners|apuestas corners hoy|apuestas
croacia argentina|apuestas cuartos eurocopa|apuestas cuotas|apuestas cuotas altas|apuestas
cuotas bajas|apuestas de 1 euro|apuestas de baloncesto|apuestas de
baloncesto hoy|apuestas de baloncesto nba|apuestas de baloncesto para hoy|apuestas de beisbol|apuestas de beisbol para hoy|apuestas de blackjack en linea|apuestas de boxeo|apuestas de
boxeo canelo|apuestas de boxeo en las vegas|apuestas de boxeo hoy|apuestas de boxeo online|apuestas de caballo|apuestas de caballos|apuestas de caballos como funciona|apuestas de caballos como se juega|apuestas de
caballos en colombia|apuestas de caballos en españa|apuestas
de caballos en linea|apuestas de caballos españa|apuestas de
caballos ganador y colocado|apuestas de caballos internacionales|apuestas de caballos juegos|apuestas de caballos online|apuestas de caballos online en venezuela|apuestas
de caballos por internet|apuestas de caballos pronosticos|apuestas de caballos pronósticos|apuestas de
carrera de caballos|apuestas de carreras de caballos|apuestas de carreras de caballos online|apuestas
de casino|apuestas de casino online|apuestas de
casino por internet|apuestas de champions league|apuestas de ciclismo|apuestas de colombia|apuestas de copa america|apuestas de corners|apuestas de
deportes en linea|apuestas de deportes online|apuestas de dinero|apuestas de
esports|apuestas de eurocopa|apuestas de europa league|apuestas de f1|apuestas de formula 1|apuestas de futbol|apuestas de
fútbol|apuestas de futbol app|apuestas de futbol argentina|apuestas de futbol colombia|apuestas de futbol en colombia|apuestas de futbol en directo|apuestas de futbol en linea|apuestas de futbol en vivo|apuestas de futbol español|apuestas de futbol gratis|apuestas de
futbol hoy|apuestas de futbol mundial|apuestas
de futbol online|apuestas de fútbol online|apuestas de futbol para hoy|apuestas de fútbol para hoy|apuestas de futbol para hoy seguras|apuestas de futbol para
mañana|apuestas de futbol peru|apuestas de futbol pronosticos|apuestas de fútbol
pronósticos|apuestas de futbol seguras|apuestas de futbol seguras para hoy|apuestas
de futbol sin dinero|apuestas de galgos|apuestas de galgos como ganar|apuestas
de galgos en directo|apuestas de galgos online|apuestas de galgos trucos|apuestas
de golf|apuestas de hockey|apuestas de hockey sobre hielo|apuestas
de hoy|apuestas de hoy seguras|apuestas de juego|apuestas de juegos|apuestas de juegos deportivos|apuestas de juegos online|apuestas de la
champions league|apuestas de la copa américa|apuestas de la eurocopa|apuestas de la europa league|apuestas de la liga|apuestas de la liga bbva|apuestas de la liga española|apuestas de la nba|apuestas de la nfl|apuestas
de la ufc|apuestas de mlb|apuestas de nba|apuestas de
nba para hoy|apuestas de partidos|apuestas de partidos de futbol|apuestas de
peleas ufc|apuestas de perros en vivo|apuestas de perros virtuales|apuestas de peru|apuestas de sistema|apuestas de sistema como funciona|apuestas
de sistema explicacion|apuestas de sistema explicación|apuestas de tenis|apuestas de tenis
de mesa|apuestas de tenis en directo|apuestas
de tenis hoy|apuestas de tenis para hoy|apuestas de tenis
pronosticos|apuestas de tenis seguras|apuestas de todo tipo|apuestas de ufc|apuestas
de ufc hoy|apuestas del boxeo|apuestas del clasico|apuestas del clasico real madrid barca|apuestas del dia|apuestas del día|apuestas del dia de
hoy|apuestas del dia deportivas|apuestas del dia futbol|apuestas del mundial|apuestas del partido de hoy|apuestas del real madrid|apuestas
del rey|apuestas del sistema|apuestas deporte|apuestas deportes|apuestas deportiva|apuestas deportivas|apuestas
deportivas 1 euro|apuestas deportivas 10 euros
gratis|apuestas deportivas 100 seguras|apuestas deportivas 1×2|apuestas deportivas android|apuestas deportivas app|apuestas deportivas apps|apuestas
deportivas argentina|apuestas deportivas argentina futbol|apuestas deportivas argentina legal|apuestas deportivas atletico de
madrid|apuestas deportivas baloncesto|apuestas deportivas barca madrid|apuestas deportivas barcelona|apuestas deportivas beisbol|apuestas deportivas bono|apuestas deportivas bono bienvenida|apuestas
deportivas bono de bienvenida|apuestas deportivas bono sin deposito|apuestas deportivas bonos de bienvenida|apuestas deportivas boxeo|apuestas deportivas caballos|apuestas deportivas calculadora|apuestas deportivas
campeon liga|apuestas deportivas casino|apuestas deportivas casino barcelona|apuestas deportivas casino online|apuestas deportivas cerca de mi|apuestas deportivas champions league|apuestas deportivas chile|apuestas deportivas ciclismo|apuestas deportivas colombia|apuestas deportivas com|apuestas deportivas com foro|apuestas deportivas com pronosticos|apuestas deportivas combinadas|apuestas deportivas combinadas para hoy|apuestas
deportivas como se juega|apuestas deportivas comparador|apuestas deportivas con bono gratis|apuestas deportivas con bonos gratis|apuestas deportivas con dinero ficticio|apuestas deportivas
con paypal|apuestas deportivas con puntos virtuales|apuestas deportivas consejos|apuestas deportivas consejos para ganar|apuestas deportivas
copa america|apuestas deportivas copa del rey|apuestas deportivas copa
libertadores|apuestas deportivas copa mundial|apuestas
deportivas corners|apuestas deportivas cual es la mejor|apuestas deportivas cuotas altas|apuestas
deportivas de baloncesto|apuestas deportivas de boxeo|apuestas
deportivas de colombia|apuestas deportivas de futbol|apuestas deportivas
de nba|apuestas deportivas de nhl|apuestas deportivas de peru|apuestas
deportivas de tenis|apuestas deportivas del dia|apuestas deportivas dinero ficticio|apuestas deportivas directo|apuestas deportivas doble oportunidad|apuestas deportivas en argentina|apuestas deportivas
en chile|apuestas deportivas en colombia|apuestas deportivas en directo|apuestas deportivas en españa|apuestas deportivas en español|apuestas deportivas en linea|apuestas deportivas en línea|apuestas deportivas
en peru|apuestas deportivas en perú|apuestas deportivas en sevilla|apuestas deportivas en uruguay|apuestas
deportivas en vivo|apuestas deportivas es|apuestas deportivas es pronosticos|apuestas deportivas españa|apuestas deportivas españolas|apuestas deportivas esports|apuestas deportivas
estadisticas|apuestas deportivas estrategias|apuestas deportivas estrategias seguras|apuestas deportivas eurocopa|apuestas deportivas europa league|apuestas deportivas f1|apuestas deportivas faciles de
ganar|apuestas deportivas formula 1|apuestas deportivas foro|apuestas deportivas
foro futbol|apuestas deportivas foro tenis|apuestas deportivas francia
argentina|apuestas deportivas futbol|apuestas deportivas fútbol|apuestas deportivas futbol argentino|apuestas deportivas futbol colombia|apuestas deportivas futbol español|apuestas
deportivas gana|apuestas deportivas ganadas|apuestas deportivas ganar
dinero seguro|apuestas deportivas gane|apuestas deportivas golf|apuestas deportivas gratis|apuestas deportivas gratis con premios|apuestas deportivas gratis hoy|apuestas deportivas gratis sin deposito|apuestas deportivas handicap|apuestas
deportivas handicap asiatico|apuestas deportivas hoy|apuestas deportivas impuestos|apuestas deportivas interior argentina|apuestas deportivas juegos olimpicos|apuestas deportivas la liga|apuestas deportivas legales|apuestas deportivas legales en colombia|apuestas deportivas
libres de impuestos|apuestas deportivas licencia españa|apuestas deportivas liga
española|apuestas deportivas listado|apuestas deportivas listado clasico|apuestas deportivas madrid|apuestas deportivas mas seguras|apuestas deportivas mejor pagadas|apuestas deportivas
mejores|apuestas deportivas mejores app|apuestas deportivas
mejores casas|apuestas deportivas mejores cuotas|apuestas deportivas mejores paginas|apuestas deportivas mexico|apuestas deportivas méxico|apuestas deportivas mlb|apuestas deportivas mlb
hoy|apuestas deportivas multiples|apuestas deportivas mundial|apuestas deportivas murcia|apuestas deportivas nba|apuestas deportivas nba hoy|apuestas deportivas nfl|apuestas deportivas nhl|apuestas deportivas nuevas|apuestas deportivas ofertas|apuestas deportivas online|apuestas deportivas online argentina|apuestas deportivas online chile|apuestas
deportivas online colombia|apuestas deportivas online en colombia|apuestas deportivas online españa|apuestas deportivas online
mexico|apuestas deportivas online paypal|apuestas deportivas online peru|apuestas deportivas online por internet|apuestas
deportivas pago paypal|apuestas deportivas para
ganar dinero|apuestas deportivas para hoy|apuestas deportivas para
hoy pronosticos|apuestas deportivas partido suspendido|apuestas
deportivas partidos de hoy|apuestas deportivas paypal|apuestas deportivas peru|apuestas deportivas
perú|apuestas deportivas peru vs ecuador|apuestas deportivas
predicciones|apuestas deportivas promociones|apuestas deportivas pronostico|apuestas deportivas pronóstico|apuestas deportivas pronostico
hoy|apuestas deportivas pronosticos|apuestas
deportivas pronósticos|apuestas deportivas pronosticos expertos|apuestas deportivas pronosticos gratis|apuestas deportivas pronosticos nba|apuestas deportivas pronosticos tenis|apuestas deportivas
que aceptan paypal|apuestas deportivas real madrid|apuestas deportivas regalo bienvenida|apuestas deportivas resultado exacto|apuestas deportivas resultados|apuestas deportivas rugby|apuestas deportivas seguras|apuestas deportivas seguras foro|apuestas deportivas seguras hoy|apuestas deportivas seguras para hoy|apuestas
deportivas seguras telegram|apuestas deportivas sevilla|apuestas deportivas simulador
eurocopa|apuestas deportivas sin deposito|apuestas deportivas sin deposito inicial|apuestas
deportivas sin dinero|apuestas deportivas sin dinero real|apuestas deportivas sin registro|apuestas deportivas stake|apuestas
deportivas stake 10|apuestas deportivas telegram españa|apuestas deportivas
tenis|apuestas deportivas tenis de mesa|apuestas deportivas tenis foro|apuestas deportivas
tenis hoy|apuestas deportivas tips|apuestas deportivas tipster|apuestas deportivas ufc|apuestas
deportivas uruguay|apuestas deportivas valencia|apuestas deportivas valencia barcelona|apuestas deportivas venezuela|apuestas deportivas virtuales|apuestas deportivas y
casino|apuestas deportivas y casino online|apuestas deportivas.com|apuestas deportivas.com foro|apuestas deportivas.es|apuestas deportivos
pronosticos|apuestas deposito minimo 1 euro|apuestas descenso a segunda|apuestas descenso a segunda b|apuestas descenso la liga|apuestas descenso primera division|apuestas
descenso segunda|apuestas dia|apuestas diarias seguras|apuestas dinero|apuestas dinero ficticio|apuestas dinero real|apuestas
dinero virtual|apuestas directas|apuestas directo|apuestas directo futbol|apuestas division de honor juvenil|apuestas dnb|apuestas doble oportunidad|apuestas doble
resultado|apuestas dobles|apuestas dobles y triples|apuestas dortmund barcelona|apuestas draft nba|apuestas draft
nfl|apuestas ecuador vs argentina|apuestas ecuador vs venezuela|apuestas egipto uruguay|apuestas el clasico|apuestas elecciones venezuela|apuestas empate|apuestas en baloncesto|apuestas
en barcelona|apuestas en beisbol|apuestas en boxeo|apuestas
en caballos|apuestas en carreras de caballos|apuestas en casino|apuestas en casino online|apuestas
en casinos|apuestas en casinos online|apuestas en chile|apuestas en ciclismo|apuestas
en colombia|apuestas en colombia de futbol|apuestas en directo|apuestas en directo futbol|apuestas
en directo pronosticos|apuestas en el futbol|apuestas en el tenis|apuestas en españa|apuestas en esports|apuestas en eventos deportivos virtuales|apuestas en golf|apuestas en juegos|apuestas en la champions league|apuestas
en la eurocopa|apuestas en la liga|apuestas en la nba|apuestas en la nfl|apuestas en las vegas
mlb|apuestas en las vegas nfl|apuestas en linea|apuestas en línea|apuestas en linea argentina|apuestas en linea boxeo|apuestas en linea chile|apuestas en linea colombia|apuestas en línea de fútbol|apuestas
en linea deportivas|apuestas en linea españa|apuestas en linea
estados unidos|apuestas en linea futbol|apuestas en linea mexico|apuestas en línea méxico|apuestas en linea mundial|apuestas en linea peru|apuestas en linea usa|apuestas
en los esports|apuestas en madrid|apuestas en méxico|apuestas en mexico online|apuestas en nba|apuestas en partidos
de futbol|apuestas en partidos de futbol en vivo|apuestas en partidos de tenis en directo|apuestas en perú|apuestas en sevilla|apuestas en sistema|apuestas en stake|apuestas en tenis|apuestas en tenis de mesa|apuestas en valencia|apuestas en vivo|apuestas en vivo argentina|apuestas en vivo casino|apuestas en vivo
futbol|apuestas en vivo fútbol|apuestas en vivo nba|apuestas
en vivo peru|apuestas en vivo tenis|apuestas en vivo
ufc|apuestas equipo mbappe|apuestas equipos de futbol|apuestas españa|apuestas españa alemania|apuestas españa alemania eurocopa|apuestas españa croacia|apuestas españa eurocopa|apuestas españa
francia|apuestas españa francia eurocopa|apuestas españa gana el mundial|apuestas españa gana eurocopa|apuestas españa gana mundial|apuestas españa georgia|apuestas españa holanda|apuestas españa inglaterra|apuestas españa inglaterra cuotas|apuestas españa
inglaterra eurocopa|apuestas españa italia|apuestas españa mundial|apuestas españa
paises bajos|apuestas español|apuestas español oviedo|apuestas espanyol barcelona|apuestas espanyol betis|apuestas espanyol villarreal|apuestas esport|apuestas esports|apuestas esports colombia|apuestas esports españa|apuestas esports fifa|apuestas esports gratis|apuestas esports lol|apuestas esports peru|apuestas
esports valorant|apuestas estadisticas|apuestas
estrategias|apuestas euro|apuestas euro copa|apuestas eurocopa|apuestas eurocopa campeon|apuestas eurocopa españa|apuestas eurocopa favoritos|apuestas eurocopa femenina|apuestas
eurocopa final|apuestas eurocopa ganador|apuestas eurocopa hoy|apuestas eurocopa sub 21|apuestas euroliga baloncesto|apuestas
euroliga pronosticos|apuestas europa league|apuestas europa league hoy|apuestas europa league
pronosticos|apuestas europa league pronósticos|apuestas euros|apuestas f1 abu dhabi|apuestas
f1 bahrein|apuestas f1 canada|apuestas f1 china|apuestas f1 cuotas|apuestas f1 hoy|apuestas
f1 las vegas|apuestas f1 miami|apuestas f1 monaco|apuestas faciles de ganar|apuestas fáciles de ganar|apuestas faciles para
ganar|apuestas favoritas|apuestas favorito champions|apuestas favoritos champions|apuestas favoritos eurocopa|apuestas favoritos mundial|apuestas fc barcelona|apuestas
final champions cuotas|apuestas final champions league|apuestas final champions peru|apuestas
final copa|apuestas final copa america|apuestas final copa
de europa|apuestas final copa del rey|apuestas final copa europa|apuestas final copa libertadores|apuestas final copa rey|apuestas final de
copa|apuestas final de copa del rey|apuestas final del mundial|apuestas final
euro|apuestas final eurocopa|apuestas final europa league|apuestas final libertadores|apuestas final mundial|apuestas final nba|apuestas final rugby|apuestas
final uefa europa league|apuestas final.mundial|apuestas finales de conferencia nfl|apuestas finales nba|apuestas fiorentina betis|apuestas formula|apuestas formula 1|apuestas fórmula 1|apuestas fórmula 1 pronósticos|apuestas formula uno|apuestas
foro|apuestas foro nba|apuestas francia argentina|apuestas
francia españa|apuestas futbol|apuestas fútbol|apuestas
futbol americano|apuestas futbol americano nfl|apuestas futbol argentina|apuestas futbol argentino|apuestas futbol champions league|apuestas futbol chile|apuestas futbol colombia|apuestas futbol consejos|apuestas futbol en directo|apuestas fútbol en directo|apuestas
futbol en vivo|apuestas fútbol en vivo|apuestas futbol españa|apuestas futbol español|apuestas fútbol español|apuestas futbol eurocopa|apuestas futbol femenino|apuestas futbol foro|apuestas futbol gratis|apuestas futbol hoy|apuestas
fútbol hoy|apuestas futbol juegos olimpicos|apuestas futbol mexico|apuestas futbol mundial|apuestas
futbol online|apuestas futbol para hoy|apuestas futbol peru|apuestas futbol pronosticos|apuestas futbol
sala|apuestas futbol telegram|apuestas futbol virtual|apuestas galgos|apuestas galgos
en directo|apuestas galgos hoy|apuestas galgos online|apuestas galgos pronosticos|apuestas
galgos trucos|apuestas gana|apuestas gana colombia|apuestas gana resultados|apuestas ganadas|apuestas ganadas hoy|apuestas ganador champions
league|apuestas ganador copa america|apuestas ganador copa del rey|apuestas ganador copa del rey baloncesto|apuestas ganador copa libertadores|apuestas
ganador de la eurocopa|apuestas ganador de la liga|apuestas
ganador del mundial|apuestas ganador eurocopa|apuestas ganador europa league|apuestas ganador f1|apuestas ganador la liga|apuestas ganador liga española|apuestas ganador
mundial|apuestas ganador mundial baloncesto|apuestas ganador
mundial f1|apuestas ganador nba|apuestas ganadores eurocopa|apuestas
ganadores mundial|apuestas ganar champions|apuestas ganar eurocopa|apuestas ganar liga|apuestas ganar mundial|apuestas ganar nba|apuestas getafe valencia|apuestas ghana uruguay|apuestas girona|apuestas girona athletic|apuestas girona betis|apuestas girona campeon de liga|apuestas girona campeon liga|apuestas girona gana la liga|apuestas
girona real madrid|apuestas girona real sociedad|apuestas
goleador eurocopa|apuestas goleadores eurocopa|apuestas goles asiaticos|apuestas golf|apuestas
golf masters|apuestas golf pga|apuestas granada barcelona|apuestas grand slam de tenis|apuestas gratis|apuestas gratis casino|apuestas gratis con premios|apuestas gratis hoy|apuestas gratis para hoy|apuestas gratis por
registro|apuestas gratis puntos|apuestas gratis regalos|apuestas gratis sin deposito|apuestas gratis sin depósito|apuestas gratis sin ingreso|apuestas gratis sports|apuestas
gratis y ganar premios|apuestas grupo a eurocopa|apuestas grupos eurocopa|apuestas handicap|apuestas handicap asiatico|apuestas handicap baloncesto|apuestas handicap como funciona|apuestas handicap
nba|apuestas handicap nfl|apuestas hipicas online|apuestas hípicas
online|apuestas hipicas venezuela|apuestas hockey|apuestas hockey hielo|apuestas
hockey patines|apuestas hockey sobre hielo|apuestas
holanda argentina|apuestas holanda vs argentina|apuestas hoy|apuestas hoy champions|apuestas hoy futbol|apuestas hoy nba|apuestas
hoy pronosticos|apuestas hoy seguras|apuestas impuestos|apuestas inglaterra paises bajos|apuestas inter
barca|apuestas inter barcelona|apuestas juego|apuestas juegos|apuestas juegos en linea|apuestas
juegos olimpicos|apuestas juegos olímpicos|apuestas juegos olimpicos baloncesto|apuestas juegos online|apuestas
juegos virtuales|apuestas jugador sevilla|apuestas jugadores nba|apuestas kings league americas|apuestas la liga|apuestas la liga española|apuestas la liga hoy|apuestas la liga santander|apuestas las vegas mlb|apuestas las vegas nba|apuestas las
vegas nfl|apuestas league of legends mundial|apuestas legal|apuestas legales|apuestas legales en colombia|apuestas
legales en españa|apuestas legales en estados unidos|apuestas legales españa|apuestas leganes betis|apuestas libertadores|apuestas licencia|apuestas liga
1 peru|apuestas liga argentina|apuestas liga bbva pronosticos|apuestas liga de campeones|apuestas liga de
campeones de baloncesto|apuestas liga de campeones de hockey|apuestas
liga españa|apuestas liga española|apuestas liga santander pronosticos|apuestas ligas de futbol|apuestas linea|apuestas linea de gol|apuestas liverpool barcelona|apuestas liverpool real
madrid|apuestas lol mundial|apuestas madrid|apuestas madrid arsenal|apuestas madrid atletico|apuestas madrid atletico champions|apuestas madrid barca|apuestas madrid barça|apuestas madrid barca hoy|apuestas madrid barca supercopa|apuestas madrid barcelona|apuestas madrid barsa|apuestas madrid bayern|apuestas madrid betis|apuestas madrid borussia|apuestas
madrid campeon champions|apuestas madrid celta|apuestas madrid city|apuestas madrid dortmund|apuestas madrid
gana la liga|apuestas madrid gana liga|apuestas madrid hoy|apuestas madrid liverpool|apuestas
madrid osasuna|apuestas madrid sevilla|apuestas madrid valencia|apuestas madrid vs arsenal|apuestas madrid vs barcelona|apuestas mallorca osasuna|apuestas mallorca real sociedad|apuestas
manchester athletic|apuestas manchester city real madrid|apuestas mas
faciles de ganar|apuestas mas seguras|apuestas mas seguras para hoy|apuestas masters
de golf|apuestas masters de tenis|apuestas maximo goleador eurocopa|apuestas maximo
goleador mundial|apuestas mejor jugador eurocopa|apuestas mejores casinos
online|apuestas mexico|apuestas méxico|apuestas mexico polonia|apuestas méxico polonia|apuestas mlb|apuestas mlb hoy|apuestas mlb las vegas|apuestas mlb para hoy|apuestas mlb pronosticos|apuestas mlb
usa|apuestas mma ufc|apuestas momios|apuestas
multiples|apuestas múltiples|apuestas multiples como funcionan|apuestas multiples el gordo|apuestas multiples futbol|apuestas mundial|apuestas mundial 2026|apuestas
mundial baloncesto|apuestas mundial balonmano|apuestas mundial brasil|apuestas mundial campeon|apuestas
mundial ciclismo|apuestas mundial clubes|apuestas mundial
de baloncesto|apuestas mundial de ciclismo|apuestas mundial de clubes|apuestas mundial de futbol|apuestas mundial de fútbol|apuestas mundial de rugby|apuestas mundial f1|apuestas mundial favoritos|apuestas mundial femenino|apuestas mundial formula 1|apuestas mundial futbol|apuestas mundial ganador|apuestas mundial lol|apuestas mundial
moto gp|apuestas mundial motogp|apuestas mundial rugby|apuestas mundial sub 17|apuestas mundiales|apuestas mundialistas|apuestas mvp eurocopa|apuestas mvp nba|apuestas mvp nfl|apuestas nacionales de
colombia|apuestas nba|apuestas nba all star|apuestas nba
campeon|apuestas nba consejos|apuestas nba esta noche|apuestas nba finals|apuestas nba gratis|apuestas nba hoy|apuestas nba
hoy jugadores|apuestas nba hoy pronosticos|apuestas nba para hoy|apuestas nba playoffs|apuestas nba pronosticos|apuestas nba pronósticos|apuestas nba pronosticos hoy|apuestas nba tipster|apuestas
nfl|apuestas nfl hoy|apuestas nfl las vegas|apuestas nfl
playoffs|apuestas nfl pronosticos|apuestas nfl pronósticos|apuestas nfl semana 4|apuestas nfl super bowl|apuestas nhl|apuestas nhl pronosticos|apuestas octavos eurocopa|apuestas
ofertas|apuestas online|apuestas online argentina|apuestas online
argentina legal|apuestas online bono|apuestas online
bono bienvenida|apuestas online boxeo|apuestas online caballos|apuestas online carreras de caballos|apuestas online casino|apuestas online champions league|apuestas online
chile|apuestas online ciclismo|apuestas online colombia|apuestas online comparativa|apuestas online con paypal|apuestas online de caballos|apuestas online deportivas|apuestas online
en argentina|apuestas online en peru|apuestas online
espana|apuestas online españa|apuestas online esports|apuestas online foro|apuestas online futbol|apuestas online futbol españa|apuestas online golf|apuestas online gratis|apuestas online gratis sin deposito|apuestas online juegos|apuestas
online mexico|apuestas online mma|apuestas online movil|apuestas online nba|apuestas online net|apuestas online nuevas|apuestas online opiniones|apuestas online paypal|apuestas online peru|apuestas online seguras|apuestas online sin dinero|apuestas online sin registro|apuestas online tenis|apuestas online ufc|apuestas online uruguay|apuestas online venezuela|apuestas open britanico golf|apuestas osasuna athletic|apuestas osasuna barcelona|apuestas osasuna real madrid|apuestas osasuna sevilla|apuestas osasuna valencia|apuestas over|apuestas over 2.5|apuestas over under|apuestas paginas|apuestas
pago anticipado|apuestas paises bajos ecuador|apuestas paises bajos inglaterra|apuestas países bajos qatar|apuestas para boxeo|apuestas para
champions league|apuestas para el clasico|apuestas para el dia de hoy|apuestas para el
mundial|apuestas para el partido de hoy|apuestas para
eurocopa|apuestas para europa league|apuestas para futbol|apuestas para ganar|apuestas para ganar dinero|apuestas para ganar dinero facil|apuestas para ganar en la ruleta|apuestas para ganar la champions|apuestas para ganar la eurocopa|apuestas para ganar la europa
league|apuestas para ganar la liga|apuestas para ganar siempre|apuestas para hacer|apuestas para hoy|apuestas para hoy de futbol|apuestas para hoy
europa league|apuestas para hoy futbol|apuestas para juegos|apuestas para la champions league|apuestas para la copa del rey|apuestas para la eurocopa|apuestas para la europa league|apuestas para
la final de la eurocopa|apuestas para la nba hoy|apuestas para los partidos de hoy|apuestas para partidos de
hoy|apuestas para ufc|apuestas partido|apuestas partido aplazado|apuestas partido
champions|apuestas partido colombia|apuestas partido españa marruecos|apuestas
partido mundial|apuestas partido suspendido|apuestas partidos|apuestas partidos champions league|apuestas partidos
csgo|apuestas partidos de futbol|apuestas partidos de futbol hoy|apuestas partidos de hoy|apuestas partidos eurocopa|apuestas partidos futbol|apuestas partidos
hoy|apuestas partidos mundial|apuestas paypal|apuestas peleas de boxeo|apuestas peru|apuestas perú|apuestas peru brasil|apuestas peru chile|apuestas peru
paraguay|apuestas peru uruguay|apuestas peru
vs chile|apuestas peru vs colombia|apuestas pichichi eurocopa|apuestas plataforma|apuestas playoff|apuestas
playoff ascenso|apuestas playoff ascenso a primera|apuestas playoff nba|apuestas playoff segunda|apuestas playoff
segunda b|apuestas playoffs nba|apuestas playoffs nfl|apuestas polonia argentina|apuestas por argentina|apuestas por internet
mexico|apuestas por internet para ganar dinero|apuestas por paypal|apuestas
por ronda boxeo|apuestas por sistema|apuestas portugal
uruguay|apuestas pre partido|apuestas predicciones|apuestas predicciones futbol|apuestas primera division|apuestas primera division españa|apuestas promociones|apuestas pronostico|apuestas pronosticos|apuestas pronosticos deportivos|apuestas pronosticos deportivos
tenis|apuestas pronosticos futbol|apuestas pronosticos gratis|apuestas pronosticos
nba|apuestas pronosticos tenis|apuestas prorroga|apuestas psg barca|apuestas psg barcelona|apuestas puntos por tarjetas|apuestas puntos
tarjetas|apuestas que aceptan paypal|apuestas que es handicap|apuestas que puedes hacer con tu novia|apuestas que siempre ganaras|apuestas que significa|apuestas quien bajara a segunda|apuestas quién bajara a
segunda|apuestas quien gana el mundial|apuestas quien gana eurocopa|apuestas quien gana la
champions|apuestas quien gana la eurocopa|apuestas quien gana la
liga|apuestas quien ganara el mundial|apuestas quién ganará el mundial|apuestas quien ganara la champions|apuestas quien ganara la eurocopa|apuestas quien ganara la liga|apuestas rayo barcelona|apuestas real madrid|apuestas real madrid arsenal|apuestas real madrid
athletic|apuestas real madrid atletico|apuestas real madrid atletico
champions|apuestas real madrid atletico de madrid|apuestas real madrid atlético de madrid|apuestas real madrid
atletico madrid|apuestas real madrid barcelona|apuestas real madrid
bayern|apuestas real madrid betis|apuestas real madrid borussia|apuestas real
madrid campeon champions|apuestas real madrid celta|apuestas real madrid champions|apuestas real madrid city|apuestas real madrid girona|apuestas real madrid hoy|apuestas real madrid liverpool|apuestas real madrid manchester
city|apuestas real madrid osasuna|apuestas real madrid real sociedad|apuestas real madrid valencia|apuestas real madrid villarreal|apuestas real madrid vs arsenal|apuestas real madrid vs atletico|apuestas real madrid vs atlético|apuestas real madrid vs
atletico madrid|apuestas real madrid vs barcelona|apuestas real madrid vs betis|apuestas real madrid vs sevilla|apuestas real
madrid vs valencia|apuestas real sociedad|apuestas real
sociedad athletic|apuestas real sociedad barcelona|apuestas real sociedad
betis|apuestas real sociedad psg|apuestas real sociedad real madrid|apuestas real sociedad valencia|apuestas recomendadas
hoy|apuestas regalo de bienvenida|apuestas registro|apuestas resultado exacto|apuestas resultados|apuestas resultados eurocopa|apuestas
retirada tenis|apuestas roma barcelona|apuestas roma sevilla|apuestas rugby|apuestas rugby
mundial|apuestas rugby world cup|apuestas ruleta seguras|apuestas segunda|apuestas segunda b|apuestas segunda division|apuestas
segunda división|apuestas segunda division b|apuestas segunda division españa|apuestas seguras|apuestas seguras baloncesto|apuestas seguras
calculadora|apuestas seguras en la ruleta|apuestas seguras eurocopa|apuestas seguras
foro|apuestas seguras futbol|apuestas seguras futbol
hoy|apuestas seguras gratis|apuestas seguras hoy|apuestas seguras hoy futbol|apuestas seguras nba|apuestas seguras nba hoy|apuestas seguras para este fin de semana|apuestas seguras para ganar dinero|apuestas seguras para
hoy|apuestas seguras para hoy fútbol|apuestas seguras para hoy pronósticos|apuestas seguras para
mañana|apuestas seguras ruleta|apuestas seguras telegram|apuestas seguras tenis|apuestas
semifinales eurocopa|apuestas senegal paises bajos|apuestas
sevilla|apuestas sevilla athletic|apuestas sevilla atletico de madrid|apuestas sevilla barcelona|apuestas sevilla betis|apuestas sevilla campeon liga|apuestas sevilla celta|apuestas sevilla gana la liga|apuestas sevilla girona|apuestas sevilla inter|apuestas sevilla jugador|apuestas sevilla juventus|apuestas
sevilla leganes|apuestas sevilla madrid|apuestas sevilla manchester united|apuestas sevilla osasuna|apuestas
sevilla real madrid|apuestas sevilla real sociedad|apuestas sevilla
roma|apuestas sevilla valencia|apuestas significa|apuestas simples
ejemplos|apuestas simples o combinadas|apuestas sin deposito|apuestas sin deposito
inicial|apuestas sin deposito minimo|apuestas sin dinero|apuestas sin dinero real|apuestas
sin empate|apuestas sin empate que significa|apuestas sin ingreso minimo|apuestas sin registro|apuestas sistema|apuestas sistema calculadora|apuestas sistema como funciona|apuestas sistema trixie|apuestas sociedad|apuestas
sorteo copa del rey|apuestas stake|apuestas stake
10|apuestas stake 10 hoy|apuestas super bowl favorito|apuestas super
rugby|apuestas supercopa españa|apuestas superliga argentina|apuestas tarjeta roja|apuestas tarjetas|apuestas tarjetas amarillas|apuestas tenis|apuestas tenis atp|apuestas tenis consejos|apuestas tenis copa davis|apuestas tenis de mesa|apuestas tenis de mesa pronosticos|apuestas tenis en vivo|apuestas tenis femenino|apuestas tenis
hoy|apuestas tenis itf|apuestas tenis pronosticos|apuestas
tenis pronósticos|apuestas tenis retirada|apuestas tenis roland garros|apuestas tenis seguras|apuestas tenis
wimbledon|apuestas tenis wta|apuestas tercera division|apuestas tercera division españa|apuestas
tipos|apuestas tips|apuestas tipster|apuestas tipster para hoy|apuestas topuria
holloway cuotas|apuestas torneos de golf|apuestas torneos de tenis|apuestas trucos|apuestas uefa champions league|apuestas uefa europa league|apuestas ufc|apuestas ufc chile|apuestas
ufc como funciona|apuestas ufc hoy|apuestas ufc ilia topuria|apuestas ufc online|apuestas ufc pronósticos|apuestas ufc telegram|apuestas
ufc topuria|apuestas under over|apuestas unionistas villarreal|apuestas uruguay|apuestas uruguay colombia|apuestas
uruguay corea|apuestas uruguay vs colombia|apuestas us open golf|apuestas
us open tenis|apuestas valencia|apuestas valencia barcelona|apuestas valencia betis|apuestas valencia madrid|apuestas valencia real madrid|apuestas valladolid barcelona|apuestas valladolid valencia|apuestas valor app|apuestas valor en directo|apuestas valor galgos|apuestas
venezuela|apuestas venezuela argentina|apuestas venezuela
bolivia|apuestas venezuela ecuador|apuestas villarreal|apuestas villarreal athletic|apuestas villarreal barcelona|apuestas villarreal
bayern|apuestas villarreal betis|apuestas villarreal liverpool|apuestas villarreal manchester|apuestas villarreal manchester united|apuestas villarreal vs real madrid|apuestas virtuales|apuestas virtuales colombia|apuestas virtuales futbol|apuestas virtuales sin dinero|apuestas vivo|apuestas vuelta a españa|apuestas vuelta españa|apuestas william hill partidos de hoy|apuestas
y casino|apuestas y casinos|apuestas y juegos de azar|apuestas y pronosticos|apuestas y pronosticos de futbol|apuestas y pronosticos deportivos|apuestas y resultados|apuestas-deportivas|apuestas-deportivas.es pronosticos|arbitro nba apuestas|argentina apuestas|argentina colombia apuestas|argentina croacia apuestas|argentina francia apuestas|argentina
mexico apuestas|argentina peru apuestas|argentina uruguay apuestas|argentina vs bolivia apuestas|argentina vs chile apuestas|argentina vs colombia apuestas|argentina vs francia apuestas|argentina vs.
colombia apuestas|asi se gana en las apuestas deportivas|asiatico apuestas|asiatico en apuestas|asiaticos apuestas|athletic barcelona
apuestas|athletic manchester united apuestas|athletic osasuna apuestas|athletic real madrid apuestas|atletico barcelona apuestas|atletico de madrid apuestas|atlético de madrid apuestas|atletico de madrid real madrid apuestas|atletico de madrid vs barcelona apuestas|atletico
madrid real madrid apuestas|atletico madrid vs real
madrid apuestas|atletico real madrid apuestas|atletico vs real madrid apuestas|avisador de cuotas apuestas|bajada de cuotas apuestas|baloncesto
apuestas|barbastro barcelona apuestas|barca apuestas|barca bayern apuestas|barca inter apuestas|barca
madrid apuestas|barça madrid apuestas|barca vs atletico apuestas|barca vs madrid apuestas|barca vs real madrid apuestas|barcelona – real madrid apuestas|barcelona apuestas|barcelona atletico apuestas|barcelona atletico de madrid apuestas|barcelona atletico madrid apuestas|barcelona betis
apuestas|barcelona casa de apuestas|barcelona inter
apuestas|barcelona psg apuestas|barcelona real madrid apuestas|barcelona
real sociedad apuestas|barcelona sevilla apuestas|barcelona
valencia apuestas|barcelona vs athletic bilbao apuestas|barcelona vs atlético madrid apuestas|barcelona vs betis apuestas|barcelona vs celta de vigo apuestas|barcelona vs
espanyol apuestas|barcelona vs girona apuestas|barcelona vs madrid apuestas|barcelona vs real madrid
apuestas|barcelona vs real sociedad apuestas|barcelona vs sevilla apuestas|barcelona vs villarreal apuestas|base de datos cuotas apuestas deportivas|bayern real madrid apuestas|beisbol apuestas|best america apuestas|bet apuestas chile|bet apuestas
en vivo|betis – chelsea apuestas|betis apuestas|betis barcelona apuestas|betis chelsea apuestas|betis madrid apuestas|betis sevilla apuestas|betsson tu sitio de apuestas
online|blog apuestas baloncesto|blog apuestas ciclismo|blog apuestas
nba|blog apuestas tenis|blog de apuestas de
tenis|bono apuestas|bono apuestas deportivas|bono
apuestas deportivas sin deposito|bono apuestas gratis|bono apuestas gratis sin deposito|bono apuestas sin deposito|bono bienvenida apuestas|bono bienvenida apuestas deportivas|bono bienvenida apuestas españa|bono bienvenida apuestas sin deposito|bono bienvenida apuestas sin depósito|bono bienvenida
casa apuestas|bono bienvenida casa de apuestas|bono bienvenida marca apuestas|bono casa apuestas|bono casa de apuestas|bono casa de apuestas sin ingreso|bono casas
de apuestas|bono de apuestas|bono de apuestas gratis sin deposito|bono de bienvenida apuestas|bono de bienvenida apuestas deportivas|bono de bienvenida casa de apuestas|bono de bienvenida
casas de apuestas|bono de casas de apuestas|bono de registro apuestas|bono de registro apuestas
deportivas|bono de registro casa de apuestas|bono gratis apuestas|bono marca apuestas|bono por
registro apuestas|bono por registro apuestas deportivas|bono por registro casa de apuestas|bono registro
apuestas|bono sin deposito apuestas|bono sin depósito apuestas|bono sin deposito apuestas
deportivas|bono sin depósito apuestas deportivas|bono sin deposito casa de apuestas|bono sin deposito marca apuestas|bono sin ingreso apuestas|bono sin ingreso apuestas deportivas|bonos apuestas|bonos apuestas colombia|bonos apuestas deportivas|bonos apuestas deportivas sin deposito|bonos apuestas gratis|bonos
apuestas sin deposito|bonos apuestas sin depósito|bonos bienvenida
apuestas|bonos bienvenida casas apuestas|bonos bienvenida casas de apuestas|bonos
casa de apuestas|bonos casas apuestas|bonos casas de apuestas|bonos casas de apuestas colombia|bonos casas de apuestas deportivas|bonos
casas de apuestas españa|bonos casas de apuestas nuevas|bonos
casas de apuestas sin deposito|bonos casas de apuestas sin depósito|bonos de apuestas|bonos de apuestas deportivas|bonos de apuestas gratis|bonos de apuestas sin deposito|bonos de bienvenida apuestas|bonos
de bienvenida apuestas deportivas|bonos de bienvenida casa de apuestas|bonos de bienvenida casas de apuestas|bonos de bienvenida de casas de apuestas|bonos de bienvenida en casas de apuestas|bonos de casas de apuestas|bonos de casas de apuestas sin deposito|bonos en casa de apuestas|bonos en casas de apuestas sin deposito|bonos gratis apuestas|bonos gratis apuestas deportivas|bonos gratis casas de apuestas|bonos gratis
sin deposito apuestas|bonos paginas de apuestas|bonos registro casas de apuestas|bonos sin deposito apuestas|bonos sin depósito apuestas|bonos sin deposito apuestas deportivas|bonos
sin deposito casas de apuestas|bot de apuestas deportivas gratis|boxeo apuestas|brasil colombia apuestas|brasil peru
apuestas|brasil vs colombia apuestas|buenas apuestas para hoy|buscador cuotas apuestas|buscador de apuestas seguras|buscador de cuotas apuestas|buscador de cuotas de apuestas|buscar
apuestas seguras|caballos apuestas|calculador de apuestas|calculador de cuotas apuestas|calculadora apuestas|calculadora apuestas combinadas|calculadora apuestas
de sistema|calculadora apuestas deportivas|calculadora apuestas deportivas seguras|calculadora apuestas multiples|calculadora apuestas segura|calculadora apuestas seguras|calculadora apuestas sistema|calculadora
apuestas yankee|calculadora arbitraje apuestas|calculadora cubrir apuestas|calculadora cuotas apuestas|calculadora de apuestas|calculadora de apuestas combinadas|calculadora de apuestas de futbol|calculadora de
apuestas de sistema|calculadora de apuestas
deportivas|calculadora de apuestas multiples|calculadora de apuestas seguras|calculadora de apuestas sistema|calculadora de apuestas surebets|calculadora
de arbitraje apuestas|calculadora de cuotas apuestas|calculadora de cuotas de apuestas|calculadora para apuestas deportivas|calculadora poisson apuestas|calculadora poisson apuestas deportivas|calculadora poisson para apuestas|calculadora scalping apuestas deportivas|calculadora sistema apuestas|calculadora stake apuestas|calculadora trading apuestas|calcular apuestas|calcular apuestas deportivas|calcular apuestas futbol|calcular
apuestas sistema|calcular cuotas apuestas|calcular cuotas apuestas combinadas|calcular cuotas apuestas
deportivas|calcular cuotas de apuestas|calcular ganancias apuestas deportivas|calcular momios apuestas|calcular probabilidad
cuota apuestas|calcular stake apuestas|calcular
unidades apuestas|calcular yield apuestas|calculo de apuestas|calculo de apuestas deportivas|cambio de cuotas apuestas|campeon champions apuestas|campeon eurocopa
apuestas|campeon liga apuestas|campeon nba apuestas|canales de apuestas gratis|carrera de caballos apuestas|carrera de caballos apuestas juego|carrera
de caballos con apuestas|carrera de galgos apuestas|carreras de
caballos apuestas|carreras de caballos apuestas
online|carreras de caballos con apuestas|carreras de
caballos juegos de apuestas|carreras de galgos apuestas|carreras de galgos apuestas
online|carreras de galgos apuestas trucos|carreras galgos apuestas|casa
apuestas argentina|casa apuestas atletico de madrid|casa apuestas barcelona|casa apuestas betis|casa apuestas bono bienvenida|casa apuestas bono
gratis|casa apuestas bono sin deposito|casa apuestas cerca
de mi|casa apuestas chile|casa apuestas colombia|casa apuestas con mejores cuotas|casa apuestas deportivas|casa apuestas españa|casa apuestas española|casa
apuestas eurocopa|casa apuestas futbol|casa apuestas mejores cuotas|casa apuestas mundial|casa
apuestas nueva|casa apuestas nuevas|casa apuestas online|casa apuestas peru|casa apuestas
valencia|casa de apuestas|casa de apuestas 10 euros gratis|casa de apuestas argentina|casa
de apuestas atletico de madrid|casa de apuestas baloncesto|casa de apuestas barcelona|casa de apuestas beisbol|casa de apuestas betis|casa de
apuestas bono|casa de apuestas bono bienvenida|casa de apuestas
bono de bienvenida|casa de apuestas bono gratis|casa de apuestas bono
por registro|casa de apuestas bono sin deposito|casa de
apuestas boxeo|casa de apuestas caballos|casa de apuestas carreras de caballos|casa de
apuestas cerca de mi|casa de apuestas cerca de mí|casa de apuestas
champions league|casa de apuestas chile|casa de apuestas ciclismo|casa de
apuestas colombia|casa de apuestas con bono
de bienvenida|casa de apuestas con bono sin deposito|casa de
apuestas con cuotas mas altas|casa de apuestas con esports|casa de apuestas con las mejores cuotas|casa de apuestas con licencia en españa|casa de apuestas con mejores cuotas|casa
de apuestas con pago anticipado|casa de apuestas con paypal|casa de apuestas
copa america|casa de apuestas de caballos|casa de apuestas de
colombia|casa de apuestas de españa|casa de apuestas de futbol|casa de apuestas de fútbol|casa de
apuestas de futbol peru|casa de apuestas de peru|casa de apuestas
del madrid|casa de apuestas del real madrid|casa de apuestas deportivas|casa de apuestas deportivas cerca de
mi|casa de apuestas deportivas en argentina|casa de apuestas deportivas en chile|casa de
apuestas deportivas en colombia|casa de apuestas deportivas en españa|casa de apuestas deportivas en madrid|casa de apuestas deportivas españa|casa de apuestas deportivas españolas|casa de apuestas deportivas madrid|casa de apuestas deportivas mexico|casa de apuestas deportivas online|casa de apuestas deportivas peru|casa de apuestas deposito 5 euros|casa de apuestas deposito minimo|casa
de apuestas deposito minimo 1 euro|casa de apuestas depósito mínimo 1 euro|casa de apuestas
en españa|casa de apuestas en linea|casa de apuestas en madrid|casa de apuestas en perú|casa de apuestas en vivo|casa de
apuestas españa|casa de apuestas españa inglaterra|casa de
apuestas española|casa de apuestas españolas|casa de apuestas esports|casa
de apuestas eurocopa|casa de apuestas europa league|casa de
apuestas f1|casa de apuestas formula 1|casa de apuestas futbol|casa de apuestas ingreso minimo|casa de apuestas ingreso minimo 1 euro|casa de
apuestas ingreso mínimo 1 euro|casa de apuestas legales|casa de apuestas legales en colombia|casa de apuestas legales en españa|casa de apuestas libertadores|casa de apuestas liga
española|casa de apuestas madrid|casa de apuestas mas segura|casa de
apuestas mejores|casa de apuestas méxico|casa de apuestas minimo 5 euros|casa de apuestas mlb|casa
de apuestas mundial|casa de apuestas nba|casa de
apuestas nfl|casa de apuestas nueva|casa de
apuestas nuevas|casa de apuestas oficial del real madrid|casa de apuestas oficial real madrid|casa de apuestas
online|casa de apuestas online argentina|casa de apuestas online chile|casa de apuestas online españa|casa de apuestas online mexico|casa de apuestas online paraguay|casa de apuestas online peru|casa de apuestas online usa|casa de apuestas online venezuela|casa de apuestas pago anticipado|casa de apuestas
para boxeo|casa de apuestas para ufc|casa de apuestas peru|casa de apuestas
perú|casa de apuestas peru online|casa de apuestas por
paypal|casa de apuestas promociones|casa de apuestas que
regalan dinero|casa de apuestas real madrid|casa de apuestas regalo de
bienvenida|casa de apuestas sevilla|casa de apuestas sin dinero|casa de apuestas sin ingreso minimo|casa de apuestas
sin licencia en españa|casa de apuestas sin minimo de
ingreso|casa de apuestas stake|casa de apuestas tenis|casa de apuestas ufc|casa
de apuestas valencia|casa de apuestas venezuela|casa de apuestas virtuales|casa de apuestas
vive la suerte|casa oficial de apuestas del real madrid|casas apuestas asiaticas|casas apuestas bono sin deposito|casas apuestas bonos sin deposito|casas apuestas caballos|casas apuestas chile|casas
apuestas ciclismo|casas apuestas con licencia|casas apuestas con licencia en españa|casas
apuestas deportivas|casas apuestas deportivas colombia|casas apuestas deportivas españa|casas apuestas deportivas españolas|casas apuestas deportivas nuevas|casas apuestas españa|casas apuestas españolas|casas apuestas esports|casas apuestas eurocopa|casas apuestas golf|casas apuestas ingreso
minimo 5 euros|casas apuestas legales|casas
apuestas legales españa|casas apuestas licencia|casas apuestas licencia españa|casas apuestas
mexico|casas apuestas mundial|casas apuestas nba|casas apuestas nuevas|casas apuestas nuevas españa|casas
apuestas ofertas|casas apuestas online|casas
apuestas paypal|casas apuestas peru|casas apuestas sin licencia|casas
apuestas tenis|casas asiaticas apuestas|casas de apuestas|casas de
apuestas 5 euros|casas de apuestas app|casas de apuestas argentinas|casas
de apuestas asiaticas|casas de apuestas baloncesto|casas de apuestas barcelona|casas de apuestas
bono bienvenida|casas de apuestas bono de bienvenida|casas de apuestas bono por registro|casas de
apuestas bono sin deposito|casas de apuestas bono sin ingreso|casas de apuestas bonos|casas de apuestas bonos de bienvenida|casas de apuestas bonos gratis|casas de apuestas bonos sin deposito|casas de apuestas boxeo|casas de apuestas caballos|casas
de apuestas carreras de caballos|casas de apuestas casino|casas
de apuestas casino online|casas de apuestas cerca de mi|casas de apuestas champions league|casas
de apuestas chile|casas de apuestas ciclismo|casas de
apuestas colombia|casas de apuestas com|casas de apuestas con app|casas de apuestas con apuestas
gratis|casas de apuestas con bono|casas de apuestas con bono de bienvenida|casas
de apuestas con bono de registro|casas de apuestas con bono por
registro|casas de apuestas con bono sin deposito|casas de apuestas con bonos|casas de apuestas con bonos
gratis|casas de apuestas con bonos sin deposito|casas de apuestas con deposito minimo|casas de apuestas con esports|casas de
apuestas con handicap asiatico|casas de apuestas con licencia|casas de apuestas con licencia
en españa|casas de apuestas con licencia españa|casas de apuestas con licencia española|casas de apuestas con mejores cuotas|casas de apuestas con pago anticipado|casas de apuestas con paypal|casas de apuestas con paypal
en perú|casas de apuestas con promociones|casas de apuestas
con ruleta en vivo|casas de apuestas copa del rey|casas de apuestas de caballos|casas de apuestas
de españa|casas de apuestas de futbol|casas de apuestas de fútbol|casas de apuestas de peru|casas de apuestas deportivas|casas de apuestas deportivas asiaticas|casas
de apuestas deportivas colombia|casas de apuestas deportivas comparativa|casas de apuestas deportivas con paypal|casas de apuestas deportivas en chile|casas de apuestas deportivas en españa|casas
de apuestas deportivas en linea|casas de apuestas deportivas en madrid|casas de apuestas deportivas en mexico|casas de
apuestas deportivas en peru|casas de apuestas deportivas en sevilla|casas de apuestas deportivas
en valencia|casas de apuestas deportivas españa|casas de
apuestas deportivas españolas|casas de apuestas deportivas legales|casas
de apuestas deportivas madrid|casas de apuestas deportivas mexico|casas de apuestas deportivas nuevas|casas de apuestas deportivas online|casas de
apuestas deportivas peru|casas de apuestas deportivas perú|casas de apuestas deposito minimo 1 euro|casas de apuestas depósito mínimo 1
euro|casas de apuestas dinero gratis|casas de apuestas en argentina|casas de
apuestas en barcelona|casas de apuestas en chile|casas de
apuestas en colombia|casas de apuestas en españa|casas de apuestas en españa online|casas de apuestas en linea|casas de apuestas en madrid|casas de apuestas en méxico|casas
de apuestas en peru|casas de apuestas en perú|casas de apuestas en sevilla|casas de
apuestas en uruguay|casas de apuestas en valencia|casas de apuestas en venezuela|casas de apuestas equipos de futbol|casas de apuestas españa|casas de apuestas españa alemania|casas
de apuestas españa inglaterra|casas de apuestas españa licencia|casas de apuestas españa nuevas|casas de apuestas
españa online|casas de apuestas española|casas de apuestas españolas|casas de apuestas españolas con licencia|casas de
apuestas españolas online|casas de apuestas esports|casas de apuestas eurocopa|casas de
apuestas eurocopa 2024|casas de apuestas europa league|casas de apuestas f1|casas de apuestas fisicas en barcelona|casas de apuestas fisicas en españa|casas de apuestas formula 1|casas de apuestas fuera de
españa|casas de apuestas futbol|casas de apuestas fútbol|casas de apuestas futbol españa|casas de apuestas ganador
eurocopa|casas de apuestas gratis|casas de apuestas ingreso minimo|casas
de apuestas ingreso minimo 1 euro|casas de apuestas ingreso minimo 5 euros|casas de apuestas inter barcelona|casas de apuestas legales|casas de
apuestas legales en colombia|casas de apuestas
legales en españa|casas de apuestas legales en mexico|casas de apuestas legales
españa|casas de apuestas legales mx|casas de apuestas licencia|casas de
apuestas licencia españa|casas de apuestas lista|casas
de apuestas madrid|casas de apuestas mas seguras|casas de apuestas mejores bonos|casas
de apuestas mejores cuotas|casas de apuestas mexico|casas
de apuestas méxico|casas de apuestas minimo 5 euros|casas de apuestas mlb|casas de apuestas
mundial|casas de apuestas mundial baloncesto|casas de apuestas mundiales|casas de apuestas nba|casas de apuestas no reguladas en españa|casas de
apuestas nueva ley|casas de apuestas nuevas|casas de apuestas nuevas en colombia|casas de apuestas nuevas en españa|casas de apuestas nuevas españa|casas de apuestas ofertas|casas de apuestas online|casas de apuestas online argentina|casas de apuestas online colombia|casas de apuestas
online deportivas|casas de apuestas online ecuador|casas
de apuestas online en argentina|casas de apuestas online en chile|casas de apuestas online en colombia|casas de apuestas online en españa|casas de
apuestas online en mexico|casas de apuestas online españa|casas de apuestas online mas fiables|casas de apuestas online mexico|casas de apuestas online nuevas|casas de apuestas online peru|casas de
apuestas online usa|casas de apuestas online venezuela|casas de
apuestas pago paypal|casas de apuestas para ufc|casas
de apuestas paypal|casas de apuestas peru bono sin deposito|casas de
apuestas presenciales en españa|casas de apuestas
QQ88 – Sân chơi cá cược trực tuyến chuyên nghiệp với hệ thống Thể thao, Live Casino, Nổ hũ, Bắn cá đa dạng. Tỷ lệ kèo cạnh tranh, giao dịch siêu tốc, hỗ trợ 24/7.
Почему пользователи выбирают площадку KRAKEN?
Маркетплейс KRAKEN заслужил доверие многочисленной аудитории благодаря сочетанию ключевых факторов.
Во-первых, это широкий и разнообразный ассортимент, представленный сотнями продавцов.
Во-вторых, интуитивно понятный интерфейс KRAKEN, который упрощает навигацию,
поиск товаров и управление заказами даже для
новых пользователей. В-третьих, продуманная система безопасных транзакций, включающая механизмы разрешения
споров (диспутов) и возможность использования условного депонирования, что минимизирует риски для обеих сторон
сделки. На KRAKEN функциональность сочетается с внимательным отношением к безопасности клиентов, что делает процесс покупок более предсказуемым, защищенным и, как следствие, популярным среди пользователей,
ценящих анонимность и надежность.
Почему пользователи выбирают площадку
KRAKEN?
Маркетплейс KRAKEN заслужил доверие многочисленной аудитории благодаря
сочетанию ключевых факторов.
Во-первых, это широкий и разнообразный ассортимент, представленный сотнями продавцов.
Во-вторых, интуитивно понятный интерфейс KRAKEN, который упрощает навигацию,
поиск товаров и управление заказами даже для новых пользователей.
В-третьих, продуманная система безопасных транзакций,
включающая механизмы разрешения споров (диспутов) и возможность
использования условного депонирования, что
минимизирует риски для обеих сторон сделки.
На KRAKEN функциональность сочетается с внимательным
отношением к безопасности клиентов, что делает процесс покупок более предсказуемым, защищенным и, как следствие, популярным среди пользователей, ценящих анонимность и надежность.
QQ88 mang đến trải nghiệm giải trí toàn diện cho bet thủ với tỷ lệ kèo hấp dẫn, thưởng minh bạch và hệ thống hỗ trợ 24/7 trên mọi thiết bị.
(10 euros gratis apuestas|10 mejores casas de apuestas|10 trucos para ganar apuestas|15 euros
gratis marca apuestas|1×2 apuestas|1×2 apuestas deportivas|1×2 apuestas que significa|1×2
en apuestas|1×2 en apuestas que significa|1×2 que significa en apuestas|5 euros gratis apuestas|9 apuestas que siempre ganaras|a partir de cuanto se declara apuestas|actividades de juegos de azar y apuestas|ad apuestas deportivas|aleksandre topuria ufc apuestas|algoritmo para ganar apuestas deportivas|america apuestas|análisis nba apuestas|aplicacion android apuestas deportivas|aplicacion apuestas
deportivas|aplicacion apuestas deportivas android|aplicación de apuestas online|aplicacion para hacer apuestas|aplicacion para hacer apuestas de futbol|aplicación para hacer apuestas de fútbol|aplicaciones apuestas deportivas android|aplicaciones apuestas deportivas gratis|aplicaciones de apuestas android|aplicaciones de apuestas de fútbol|aplicaciones de apuestas deportivas|aplicaciones de
apuestas deportivas peru|aplicaciones de apuestas deportivas
perú|aplicaciones de apuestas en colombia|aplicaciones de apuestas gratis|aplicaciones
de apuestas online|aplicaciones de apuestas seguras|aplicaciones de apuestas sin dinero|aplicaciones para hacer apuestas|apostar seguro apuestas deportivas|app android apuestas
deportivas|app apuestas|app apuestas android|app apuestas de futbol|app apuestas deportivas|app apuestas deportivas android|app apuestas deportivas argentina|app
apuestas deportivas colombia|app apuestas deportivas ecuador|app apuestas deportivas
españa|app apuestas deportivas gratis|app apuestas entre amigos|app apuestas
futbol|app apuestas gratis|app apuestas sin dinero|app casa de apuestas|app casas de apuestas|app control apuestas|app de apuestas|app de apuestas
android|app de apuestas casino|app de apuestas colombia|app de apuestas con bono
de bienvenida|app de apuestas de futbol|app de apuestas deportivas|app
de apuestas deportivas android|app de apuestas deportivas argentina|app de apuestas deportivas colombia|app de
apuestas deportivas en españa|app de apuestas deportivas peru|app de apuestas deportivas perú|app de apuestas deportivas sin dinero|app de apuestas ecuador|app de apuestas en colombia|app de apuestas
en españa|app de apuestas en venezuela|app de apuestas futbol|app de apuestas gratis|app
de apuestas online|app de apuestas para android|app de
apuestas para ganar dinero|app de apuestas peru|app de apuestas reales|app de casas de apuestas|app marca apuestas android|app moviles de apuestas|app para apuestas|app para apuestas
de futbol|app para apuestas deportivas|app para apuestas deportivas en español|app para
ganar apuestas deportivas|app para hacer apuestas|app para hacer apuestas deportivas|app para hacer apuestas
entre amigos|app para llevar control de apuestas|app pronosticos apuestas
deportivas|app versus apuestas|apps apuestas mundial|apps de apuestas|apps de apuestas con bono de bienvenida|apps de apuestas de futbol|apps de apuestas deportivas peru|apps de
apuestas mexico|apps para apuestas|aprender a hacer apuestas deportivas|aprender hacer apuestas deportivas|apuesta del dia apuestas deportivas|apuestas 10 euros gratis|apuestas 100
seguras|apuestas 1×2|apuestas 1X2|apuestas 2 division|apuestas 3 division|apuestas a caballos|apuestas a carreras de caballos|apuestas a colombia|apuestas a
corners|apuestas a ganar|apuestas a jugadores nba|apuestas
a la baja|apuestas a la nfl|apuestas al barcelona|apuestas al dia|apuestas al empate|apuestas al mundial|apuestas al tenis wta|apuestas alaves barcelona|apuestas alcaraz hoy|apuestas alemania españa|apuestas alonso campeon del mundo|apuestas altas y bajas|apuestas altas y bajas nfl|apuestas
ambos equipos marcan|apuestas america|apuestas android|apuestas
anillo nba|apuestas antes del mundial|apuestas anticipadas|apuestas anticipadas nba|apuestas apps|apuestas arabia
argentina|apuestas argentina|apuestas argentina campeon del mundo|apuestas argentina canada|apuestas argentina colombia|apuestas argentina croacia|apuestas
argentina españa|apuestas argentina francia|apuestas argentina francia
cuanto paga|apuestas argentina francia mundial|apuestas argentina gana el mundial|apuestas argentina
gana mundial|apuestas argentina holanda|apuestas argentina mexico|apuestas
argentina méxico|apuestas argentina mundial|apuestas argentina
online|apuestas argentina paises bajos|apuestas argentina polonia|apuestas argentina
uruguay|apuestas argentina vs australia|apuestas argentina vs colombia|apuestas argentina vs francia|apuestas argentina
vs peru|apuestas argentinas|apuestas arsenal real madrid|apuestas ascenso a primera
division|apuestas ascenso a segunda|apuestas asiaticas|apuestas asiatico|apuestas athletic|apuestas athletic atletico|apuestas
athletic barça|apuestas athletic barcelona|apuestas athletic betis|apuestas athletic manchester|apuestas athletic manchester united|apuestas athletic osasuna|apuestas athletic real|apuestas athletic real
madrid|apuestas athletic real sociedad|apuestas athletic real sociedad
final|apuestas athletic roma|apuestas athletic sevilla|apuestas athletic valencia|apuestas atletico|apuestas atletico barcelona|apuestas atletico barsa|apuestas atletico campeon champions|apuestas atletico campeon de liga|apuestas
atlético copenhague|apuestas atletico de madrid|apuestas atlético de madrid|apuestas atletico de madrid barcelona|apuestas atletico de madrid gana la liga|apuestas atletico de
madrid real madrid|apuestas atlético de madrid
real madrid|apuestas atletico de madrid vs barcelona|apuestas atletico madrid|apuestas atletico madrid real
madrid|apuestas atletico madrid vs barcelona|apuestas atletico real madrid|apuestas
atletico real madrid champions|apuestas atletismo|apuestas
bajas|apuestas baloncesto|apuestas baloncesto acb|apuestas baloncesto handicap|apuestas baloncesto
hoy|apuestas baloncesto juegos olimpicos|apuestas baloncesto nba|apuestas baloncesto pronostico|apuestas baloncesto
pronósticos|apuestas baloncesto prorroga|apuestas barca|apuestas barca athletic|apuestas barca atletico|apuestas barca bayern|apuestas barca bayern munich|apuestas
barca girona|apuestas barca hoy|apuestas barça hoy|apuestas barca inter|apuestas barca juventus|apuestas barca madrid|apuestas barça madrid|apuestas barca real madrid|apuestas barca vs
juve|apuestas barca vs madrid|apuestas barca vs psg|apuestas barcelona|apuestas barcelona
alaves|apuestas barcelona athletic|apuestas barcelona atletico|apuestas barcelona atletico de madrid|apuestas barcelona atlético de madrid|apuestas barcelona atletico madrid|apuestas barcelona bayern|apuestas barcelona betis|apuestas barcelona
campeon de liga|apuestas barcelona celta|apuestas barcelona espanyol|apuestas barcelona gana la champions|apuestas barcelona girona|apuestas barcelona granada|apuestas barcelona hoy|apuestas barcelona inter|apuestas barcelona madrid|apuestas barcelona osasuna|apuestas barcelona psg|apuestas barcelona real madrid|apuestas barcelona real sociedad|apuestas barcelona sevilla|apuestas barcelona valencia|apuestas barcelona villarreal|apuestas barcelona vs atletico
madrid|apuestas barcelona vs madrid|apuestas barcelona vs real madrid|apuestas barsa madrid|apuestas basket hoy|apuestas bayern barcelona|apuestas bayern vs barcelona|apuestas beisbol|apuestas béisbol|apuestas beisbol mlb|apuestas beisbol
pronosticos|apuestas beisbol venezolano|apuestas betis|apuestas betis – chelsea|apuestas
betis barcelona|apuestas betis chelsea|apuestas betis fiorentina|apuestas
betis girona|apuestas betis madrid|apuestas betis mallorca|apuestas betis
real madrid|apuestas betis real sociedad|apuestas betis sevilla|apuestas betis valencia|apuestas betis valladolid|apuestas betis vs valencia|apuestas betplay hoy colombia|apuestas betsson peru|apuestas bienvenida|apuestas billar online|apuestas bolivia vs colombia|apuestas bono|apuestas bono bienvenida|apuestas bono de
bienvenida|apuestas bono de bienvenida sin deposito|apuestas bono
gratis|apuestas bono sin deposito|apuestas bonos sin deposito|apuestas borussia real madrid|apuestas boxeo|apuestas boxeo de campeonato|apuestas boxeo españa|apuestas boxeo español|apuestas boxeo femenino olimpiadas|apuestas boxeo
hoy|apuestas boxeo online|apuestas brasil colombia|apuestas brasil peru|apuestas brasil uruguay|apuestas
brasil vs colombia|apuestas brasil vs peru|apuestas caballos|apuestas caballos colocado|apuestas caballos españa|apuestas caballos hipodromo|apuestas caballos hoy|apuestas caballos madrid|apuestas
caballos online|apuestas caballos sanlucar de barrameda|apuestas
caballos zarzuela|apuestas calculador|apuestas campeon|apuestas
campeon champions|apuestas campeón champions|apuestas campeon champions 2025|apuestas campeon champions league|apuestas
campeon conference league|apuestas campeon copa america|apuestas
campeon copa del rey|apuestas campeon de champions|apuestas
campeon de la champions|apuestas campeon de liga|apuestas campeon del mundo|apuestas
campeon eurocopa|apuestas campeón eurocopa|apuestas campeon europa
league|apuestas campeon f1|apuestas campeon f1 2025|apuestas campeon formula 1|apuestas campeon libertadores|apuestas campeon liga|apuestas campeon liga bbva|apuestas campeon liga española|apuestas campeon liga santander|apuestas campeon motogp 2025|apuestas
campeon mundial|apuestas campeón mundial|apuestas campeon mundial
baloncesto|apuestas campeon nba|apuestas campeón nba|apuestas campeon premier|apuestas
campeon premier league|apuestas campeon roland garros|apuestas campeonato f1|apuestas
campeonatos de futbol|apuestas carrera de caballos|apuestas carrera de caballos hoy|apuestas carrera de caballos nocturnas|apuestas carrera de galgos fin de semana|apuestas carrera de galgos hoy|apuestas carrera de galgos nocturnas|apuestas carreras caballos|apuestas
carreras caballos sanlucar|apuestas carreras de caballos|apuestas carreras de caballos en directo|apuestas carreras de caballos en vivo|apuestas carreras
de caballos españa|apuestas carreras de caballos hoy|apuestas carreras de caballos nacionales|apuestas carreras de caballos
nocturnas|apuestas carreras de caballos online|apuestas
carreras de caballos sanlucar|apuestas carreras de caballos sanlúcar|apuestas carreras de galgos|apuestas carreras de galgos en vivo|apuestas carreras de galgos
nocturnas|apuestas carreras de galgos pre partido|apuestas casino|apuestas casino
barcelona|apuestas casino futbol|apuestas casino gran madrid|apuestas casino gratis|apuestas
casino madrid|apuestas casino online|apuestas casino online argentina|apuestas casinos|apuestas
casinos online|apuestas celta|apuestas celta barcelona|apuestas celta
betis|apuestas celta eibar|apuestas celta espanyol|apuestas celta
granada|apuestas celta madrid|apuestas celta manchester|apuestas celta real
madrid|apuestas champion league|apuestas champions foro|apuestas champions hoy|apuestas champions league|apuestas champions league – pronósticos|apuestas champions league 2025|apuestas champions league hoy|apuestas champions league pronosticos|apuestas
champions league pronósticos|apuestas champions pronosticos|apuestas chelsea barcelona|apuestas chelsea betis|apuestas chile|apuestas chile peru|apuestas chile venezuela|apuestas chile vs colombia|apuestas chile
vs uruguay|apuestas ciclismo|apuestas ciclismo
en vivo|apuestas ciclismo femenino|apuestas ciclismo
tour francia|apuestas ciclismo vuelta|apuestas ciclismo vuelta
a españa|apuestas ciclismo vuelta españa|apuestas
city madrid|apuestas city real madrid|apuestas clasico|apuestas clasico español|apuestas clasico
real madrid barcelona|apuestas clasificacion mundial|apuestas colombia|apuestas colombia argentina|apuestas colombia brasil|apuestas colombia paraguay|apuestas colombia
uruguay|apuestas colombia vs argentina|apuestas colombia vs brasil|apuestas combinadas|apuestas
combinadas como funcionan|apuestas combinadas de futbol|apuestas combinadas
de fútbol|apuestas combinadas foro|apuestas combinadas futbol|apuestas combinadas hoy|apuestas combinadas mismo partido|apuestas combinadas
mundial|apuestas combinadas nba|apuestas combinadas
para esta semana|apuestas combinadas para hoy|apuestas
combinadas para mañana|apuestas combinadas pronosticos|apuestas combinadas recomendadas|apuestas combinadas seguras|apuestas combinadas seguras
para hoy|apuestas combinadas seguras para mañana|apuestas como ganar|apuestas comparador|apuestas con bono
de bienvenida|apuestas con dinero ficticio|apuestas
con dinero real|apuestas con dinero virtual|apuestas con handicap|apuestas con handicap asiatico|apuestas con handicap baloncesto|apuestas con mas probabilidades de ganar|apuestas
con paypal|apuestas con tarjeta de credito|apuestas con tarjeta de debito|apuestas consejos|apuestas copa|apuestas
copa africa|apuestas copa america|apuestas copa américa|apuestas copa argentina|apuestas copa brasil|apuestas copa davis|apuestas copa de europa|apuestas copa del mundo|apuestas copa del
rey|apuestas copa del rey baloncesto|apuestas copa del rey final|apuestas
copa del rey futbol|apuestas copa del rey ganador|apuestas copa del
rey hoy|apuestas copa del rey pronosticos|apuestas copa del rey pronósticos|apuestas copa europa|apuestas copa italia|apuestas copa libertadores|apuestas copa mundial de hockey|apuestas copa rey|apuestas copa
sudamericana|apuestas corners|apuestas corners hoy|apuestas croacia argentina|apuestas cuartos eurocopa|apuestas cuotas|apuestas cuotas altas|apuestas cuotas bajas|apuestas de 1 euro|apuestas de baloncesto|apuestas de
baloncesto hoy|apuestas de baloncesto nba|apuestas de baloncesto para hoy|apuestas de beisbol|apuestas de beisbol para hoy|apuestas de blackjack en linea|apuestas de boxeo|apuestas de
boxeo canelo|apuestas de boxeo en las vegas|apuestas de boxeo hoy|apuestas de
boxeo online|apuestas de caballo|apuestas de caballos|apuestas de caballos como funciona|apuestas de caballos como se juega|apuestas de caballos
en colombia|apuestas de caballos en españa|apuestas de caballos en linea|apuestas de caballos españa|apuestas de caballos ganador y colocado|apuestas de caballos internacionales|apuestas de caballos juegos|apuestas de caballos
online|apuestas de caballos online en venezuela|apuestas de caballos por internet|apuestas de caballos pronosticos|apuestas de caballos pronósticos|apuestas
de carrera de caballos|apuestas de carreras de caballos|apuestas de carreras
de caballos online|apuestas de casino|apuestas de casino online|apuestas de
casino por internet|apuestas de champions league|apuestas de ciclismo|apuestas de colombia|apuestas de copa america|apuestas de corners|apuestas de deportes en linea|apuestas de deportes online|apuestas
de dinero|apuestas de esports|apuestas de eurocopa|apuestas de europa league|apuestas de f1|apuestas de formula 1|apuestas de futbol|apuestas de fútbol|apuestas de
futbol app|apuestas de futbol argentina|apuestas de futbol colombia|apuestas de futbol en colombia|apuestas de futbol en directo|apuestas de futbol en linea|apuestas de
futbol en vivo|apuestas de futbol español|apuestas de futbol gratis|apuestas de
futbol hoy|apuestas de futbol mundial|apuestas de futbol online|apuestas de fútbol online|apuestas de futbol para hoy|apuestas de fútbol para hoy|apuestas
de futbol para hoy seguras|apuestas de futbol para mañana|apuestas de futbol peru|apuestas de futbol pronosticos|apuestas de fútbol pronósticos|apuestas de futbol seguras|apuestas de
futbol seguras para hoy|apuestas de futbol sin dinero|apuestas de galgos|apuestas de galgos como ganar|apuestas
de galgos en directo|apuestas de galgos online|apuestas de galgos trucos|apuestas de golf|apuestas de hockey|apuestas
de hockey sobre hielo|apuestas de hoy|apuestas de hoy seguras|apuestas de juego|apuestas de juegos|apuestas
de juegos deportivos|apuestas de juegos online|apuestas de la champions league|apuestas de la
copa américa|apuestas de la eurocopa|apuestas de la europa league|apuestas de la liga|apuestas de la
liga bbva|apuestas de la liga española|apuestas de la nba|apuestas de la nfl|apuestas de la ufc|apuestas de mlb|apuestas de nba|apuestas de nba para hoy|apuestas de partidos|apuestas de partidos de futbol|apuestas de peleas ufc|apuestas de perros en vivo|apuestas de perros virtuales|apuestas de peru|apuestas de
sistema|apuestas de sistema como funciona|apuestas de sistema explicacion|apuestas de sistema explicación|apuestas de tenis|apuestas de tenis de mesa|apuestas de tenis en directo|apuestas de tenis
hoy|apuestas de tenis para hoy|apuestas de tenis pronosticos|apuestas de tenis seguras|apuestas de todo tipo|apuestas de ufc|apuestas de ufc hoy|apuestas del boxeo|apuestas del clasico|apuestas del clasico real madrid barca|apuestas del dia|apuestas del
día|apuestas del dia de hoy|apuestas del dia deportivas|apuestas del dia futbol|apuestas del mundial|apuestas
del partido de hoy|apuestas del real madrid|apuestas del rey|apuestas del sistema|apuestas deporte|apuestas
deportes|apuestas deportiva|apuestas deportivas|apuestas deportivas 1 euro|apuestas deportivas 10 euros gratis|apuestas deportivas 100 seguras|apuestas deportivas 1×2|apuestas deportivas android|apuestas
deportivas app|apuestas deportivas apps|apuestas deportivas argentina|apuestas deportivas argentina futbol|apuestas
deportivas argentina legal|apuestas deportivas atletico de madrid|apuestas deportivas baloncesto|apuestas deportivas
barca madrid|apuestas deportivas barcelona|apuestas deportivas beisbol|apuestas deportivas bono|apuestas deportivas bono bienvenida|apuestas deportivas bono de bienvenida|apuestas deportivas bono
sin deposito|apuestas deportivas bonos de bienvenida|apuestas deportivas boxeo|apuestas deportivas caballos|apuestas deportivas calculadora|apuestas deportivas campeon liga|apuestas
deportivas casino|apuestas deportivas casino
barcelona|apuestas deportivas casino online|apuestas deportivas cerca de
mi|apuestas deportivas champions league|apuestas deportivas chile|apuestas deportivas ciclismo|apuestas deportivas colombia|apuestas deportivas com|apuestas deportivas com foro|apuestas deportivas com pronosticos|apuestas deportivas combinadas|apuestas deportivas combinadas para hoy|apuestas deportivas como se juega|apuestas deportivas comparador|apuestas deportivas con bono gratis|apuestas deportivas
con bonos gratis|apuestas deportivas con dinero ficticio|apuestas deportivas con paypal|apuestas
deportivas con puntos virtuales|apuestas deportivas consejos|apuestas deportivas consejos para ganar|apuestas deportivas copa america|apuestas deportivas copa del
rey|apuestas deportivas copa libertadores|apuestas deportivas copa
mundial|apuestas deportivas corners|apuestas deportivas
cual es la mejor|apuestas deportivas cuotas altas|apuestas deportivas de baloncesto|apuestas deportivas
de boxeo|apuestas deportivas de colombia|apuestas deportivas de futbol|apuestas
deportivas de nba|apuestas deportivas de nhl|apuestas deportivas de peru|apuestas deportivas de tenis|apuestas
deportivas del dia|apuestas deportivas dinero ficticio|apuestas deportivas directo|apuestas deportivas
doble oportunidad|apuestas deportivas en argentina|apuestas deportivas en chile|apuestas deportivas en colombia|apuestas deportivas en directo|apuestas deportivas en españa|apuestas deportivas en español|apuestas deportivas en linea|apuestas deportivas en línea|apuestas deportivas en peru|apuestas deportivas en perú|apuestas deportivas en sevilla|apuestas deportivas en uruguay|apuestas deportivas
en vivo|apuestas deportivas es|apuestas deportivas es pronosticos|apuestas
deportivas españa|apuestas deportivas españolas|apuestas
deportivas esports|apuestas deportivas estadisticas|apuestas deportivas estrategias|apuestas deportivas
estrategias seguras|apuestas deportivas eurocopa|apuestas
deportivas europa league|apuestas deportivas f1|apuestas
deportivas faciles de ganar|apuestas deportivas formula 1|apuestas deportivas foro|apuestas deportivas foro futbol|apuestas deportivas foro tenis|apuestas deportivas francia
argentina|apuestas deportivas futbol|apuestas deportivas fútbol|apuestas deportivas futbol argentino|apuestas deportivas futbol colombia|apuestas deportivas futbol español|apuestas deportivas gana|apuestas
deportivas ganadas|apuestas deportivas ganar dinero seguro|apuestas deportivas gane|apuestas deportivas golf|apuestas deportivas gratis|apuestas deportivas gratis con premios|apuestas deportivas gratis hoy|apuestas deportivas
gratis sin deposito|apuestas deportivas handicap|apuestas deportivas handicap asiatico|apuestas deportivas hoy|apuestas deportivas impuestos|apuestas deportivas interior argentina|apuestas deportivas
juegos olimpicos|apuestas deportivas la liga|apuestas deportivas legales|apuestas deportivas legales en colombia|apuestas deportivas libres
de impuestos|apuestas deportivas licencia españa|apuestas deportivas liga española|apuestas deportivas listado|apuestas deportivas listado clasico|apuestas deportivas madrid|apuestas
deportivas mas seguras|apuestas deportivas mejor pagadas|apuestas deportivas mejores|apuestas deportivas mejores app|apuestas
deportivas mejores casas|apuestas deportivas mejores cuotas|apuestas deportivas mejores
paginas|apuestas deportivas mexico|apuestas deportivas méxico|apuestas deportivas mlb|apuestas deportivas
mlb hoy|apuestas deportivas multiples|apuestas deportivas mundial|apuestas deportivas murcia|apuestas deportivas
nba|apuestas deportivas nba hoy|apuestas deportivas nfl|apuestas deportivas nhl|apuestas deportivas
nuevas|apuestas deportivas ofertas|apuestas deportivas
online|apuestas deportivas online argentina|apuestas deportivas online chile|apuestas deportivas online colombia|apuestas deportivas online en colombia|apuestas deportivas online españa|apuestas deportivas online mexico|apuestas deportivas
online paypal|apuestas deportivas online peru|apuestas deportivas online por internet|apuestas deportivas pago paypal|apuestas deportivas para ganar dinero|apuestas deportivas para hoy|apuestas deportivas
para hoy pronosticos|apuestas deportivas partido suspendido|apuestas deportivas partidos de
hoy|apuestas deportivas paypal|apuestas deportivas peru|apuestas deportivas perú|apuestas
deportivas peru vs ecuador|apuestas deportivas predicciones|apuestas deportivas promociones|apuestas deportivas pronostico|apuestas deportivas pronóstico|apuestas deportivas pronostico hoy|apuestas
deportivas pronosticos|apuestas deportivas pronósticos|apuestas deportivas pronosticos expertos|apuestas deportivas pronosticos gratis|apuestas deportivas pronosticos nba|apuestas deportivas pronosticos tenis|apuestas deportivas que aceptan paypal|apuestas deportivas real madrid|apuestas deportivas regalo bienvenida|apuestas deportivas resultado exacto|apuestas deportivas resultados|apuestas deportivas rugby|apuestas
deportivas seguras|apuestas deportivas seguras foro|apuestas deportivas seguras hoy|apuestas deportivas seguras
para hoy|apuestas deportivas seguras telegram|apuestas deportivas sevilla|apuestas deportivas simulador eurocopa|apuestas deportivas sin deposito|apuestas deportivas sin deposito inicial|apuestas deportivas sin dinero|apuestas deportivas sin dinero real|apuestas deportivas
sin registro|apuestas deportivas stake|apuestas deportivas stake 10|apuestas deportivas telegram españa|apuestas deportivas tenis|apuestas deportivas tenis de mesa|apuestas deportivas tenis foro|apuestas deportivas tenis hoy|apuestas deportivas tips|apuestas deportivas tipster|apuestas deportivas ufc|apuestas deportivas uruguay|apuestas deportivas valencia|apuestas deportivas valencia barcelona|apuestas deportivas venezuela|apuestas deportivas virtuales|apuestas deportivas
y casino|apuestas deportivas y casino online|apuestas deportivas.com|apuestas deportivas.com foro|apuestas
deportivas.es|apuestas deportivos pronosticos|apuestas deposito
minimo 1 euro|apuestas descenso a segunda|apuestas
descenso a segunda b|apuestas descenso la liga|apuestas descenso primera division|apuestas descenso segunda|apuestas dia|apuestas diarias
seguras|apuestas dinero|apuestas dinero ficticio|apuestas
dinero real|apuestas dinero virtual|apuestas directas|apuestas directo|apuestas directo futbol|apuestas division de
honor juvenil|apuestas dnb|apuestas doble oportunidad|apuestas doble resultado|apuestas
dobles|apuestas dobles y triples|apuestas dortmund
barcelona|apuestas draft nba|apuestas draft nfl|apuestas
ecuador vs argentina|apuestas ecuador vs venezuela|apuestas egipto uruguay|apuestas el clasico|apuestas
elecciones venezuela|apuestas empate|apuestas en baloncesto|apuestas
en barcelona|apuestas en beisbol|apuestas en boxeo|apuestas en caballos|apuestas en carreras
de caballos|apuestas en casino|apuestas en casino online|apuestas en casinos|apuestas en casinos online|apuestas en chile|apuestas
en ciclismo|apuestas en colombia|apuestas en colombia de futbol|apuestas en directo|apuestas en directo futbol|apuestas en directo pronosticos|apuestas en el futbol|apuestas en el tenis|apuestas en españa|apuestas en esports|apuestas en eventos
deportivos virtuales|apuestas en golf|apuestas en juegos|apuestas
en la champions league|apuestas en la eurocopa|apuestas en la liga|apuestas en la nba|apuestas en la nfl|apuestas en las vegas mlb|apuestas
en las vegas nfl|apuestas en linea|apuestas en línea|apuestas en linea argentina|apuestas en linea
boxeo|apuestas en linea chile|apuestas en linea colombia|apuestas en línea de fútbol|apuestas en linea deportivas|apuestas en linea españa|apuestas en linea estados
unidos|apuestas en linea futbol|apuestas en linea mexico|apuestas
en línea méxico|apuestas en linea mundial|apuestas en linea peru|apuestas en linea usa|apuestas
en los esports|apuestas en madrid|apuestas en méxico|apuestas
en mexico online|apuestas en nba|apuestas en partidos de
futbol|apuestas en partidos de futbol en vivo|apuestas en partidos de tenis en directo|apuestas
en perú|apuestas en sevilla|apuestas en sistema|apuestas en stake|apuestas en tenis|apuestas en tenis de mesa|apuestas en valencia|apuestas en vivo|apuestas en vivo argentina|apuestas en vivo casino|apuestas en vivo futbol|apuestas
en vivo fútbol|apuestas en vivo nba|apuestas en vivo
peru|apuestas en vivo tenis|apuestas en vivo ufc|apuestas equipo
mbappe|apuestas equipos de futbol|apuestas españa|apuestas españa alemania|apuestas españa
alemania eurocopa|apuestas españa croacia|apuestas españa eurocopa|apuestas españa
francia|apuestas españa francia eurocopa|apuestas españa gana
el mundial|apuestas españa gana eurocopa|apuestas españa gana
mundial|apuestas españa georgia|apuestas españa holanda|apuestas españa
inglaterra|apuestas españa inglaterra cuotas|apuestas
españa inglaterra eurocopa|apuestas españa italia|apuestas españa mundial|apuestas españa paises bajos|apuestas español|apuestas español oviedo|apuestas espanyol barcelona|apuestas espanyol betis|apuestas espanyol villarreal|apuestas esport|apuestas esports|apuestas esports colombia|apuestas esports españa|apuestas
esports fifa|apuestas esports gratis|apuestas esports lol|apuestas esports peru|apuestas esports valorant|apuestas
estadisticas|apuestas estrategias|apuestas euro|apuestas euro copa|apuestas eurocopa|apuestas eurocopa campeon|apuestas eurocopa españa|apuestas eurocopa favoritos|apuestas eurocopa femenina|apuestas eurocopa final|apuestas
eurocopa ganador|apuestas eurocopa hoy|apuestas eurocopa sub 21|apuestas euroliga baloncesto|apuestas euroliga pronosticos|apuestas europa league|apuestas europa league hoy|apuestas europa league pronosticos|apuestas europa league pronósticos|apuestas euros|apuestas f1 abu
dhabi|apuestas f1 bahrein|apuestas f1 canada|apuestas
f1 china|apuestas f1 cuotas|apuestas f1 hoy|apuestas f1
las vegas|apuestas f1 miami|apuestas f1 monaco|apuestas faciles de ganar|apuestas fáciles de ganar|apuestas faciles para ganar|apuestas favoritas|apuestas
favorito champions|apuestas favoritos champions|apuestas favoritos eurocopa|apuestas favoritos mundial|apuestas
fc barcelona|apuestas final champions cuotas|apuestas final champions league|apuestas final
champions peru|apuestas final copa|apuestas final copa america|apuestas final copa de europa|apuestas final copa
del rey|apuestas final copa europa|apuestas
final copa libertadores|apuestas final copa rey|apuestas final de copa|apuestas final de
copa del rey|apuestas final del mundial|apuestas final euro|apuestas final eurocopa|apuestas final europa league|apuestas final libertadores|apuestas final mundial|apuestas final nba|apuestas
final rugby|apuestas final uefa europa league|apuestas final.mundial|apuestas finales de conferencia
nfl|apuestas finales nba|apuestas fiorentina betis|apuestas formula|apuestas formula 1|apuestas fórmula 1|apuestas fórmula 1 pronósticos|apuestas formula uno|apuestas foro|apuestas foro nba|apuestas francia argentina|apuestas
francia españa|apuestas futbol|apuestas fútbol|apuestas futbol americano|apuestas futbol americano nfl|apuestas futbol
argentina|apuestas futbol argentino|apuestas futbol champions league|apuestas futbol chile|apuestas
futbol colombia|apuestas futbol consejos|apuestas futbol en directo|apuestas fútbol en directo|apuestas futbol en vivo|apuestas fútbol en vivo|apuestas futbol españa|apuestas futbol
español|apuestas fútbol español|apuestas futbol eurocopa|apuestas futbol femenino|apuestas futbol
foro|apuestas futbol gratis|apuestas futbol hoy|apuestas fútbol hoy|apuestas futbol juegos olimpicos|apuestas futbol mexico|apuestas futbol mundial|apuestas futbol
online|apuestas futbol para hoy|apuestas futbol peru|apuestas futbol pronosticos|apuestas futbol sala|apuestas futbol
telegram|apuestas futbol virtual|apuestas galgos|apuestas galgos en directo|apuestas galgos hoy|apuestas galgos
online|apuestas galgos pronosticos|apuestas galgos trucos|apuestas gana|apuestas gana colombia|apuestas gana resultados|apuestas ganadas|apuestas
ganadas hoy|apuestas ganador champions league|apuestas ganador copa america|apuestas ganador copa del rey|apuestas ganador copa del rey
baloncesto|apuestas ganador copa libertadores|apuestas ganador de la eurocopa|apuestas ganador
de la liga|apuestas ganador del mundial|apuestas ganador eurocopa|apuestas
ganador europa league|apuestas ganador f1|apuestas ganador la liga|apuestas ganador liga
española|apuestas ganador mundial|apuestas ganador mundial baloncesto|apuestas ganador mundial f1|apuestas ganador nba|apuestas
ganadores eurocopa|apuestas ganadores mundial|apuestas ganar champions|apuestas ganar eurocopa|apuestas ganar liga|apuestas ganar
mundial|apuestas ganar nba|apuestas getafe valencia|apuestas ghana uruguay|apuestas girona|apuestas girona athletic|apuestas
girona betis|apuestas girona campeon de liga|apuestas girona campeon liga|apuestas girona gana la liga|apuestas girona real madrid|apuestas girona real sociedad|apuestas goleador eurocopa|apuestas
goleadores eurocopa|apuestas goles asiaticos|apuestas golf|apuestas golf masters|apuestas golf pga|apuestas granada barcelona|apuestas grand slam de tenis|apuestas gratis|apuestas gratis casino|apuestas gratis con premios|apuestas gratis
hoy|apuestas gratis para hoy|apuestas gratis por registro|apuestas gratis
puntos|apuestas gratis regalos|apuestas gratis sin deposito|apuestas gratis sin depósito|apuestas gratis sin ingreso|apuestas gratis sports|apuestas gratis y ganar premios|apuestas grupo a eurocopa|apuestas grupos eurocopa|apuestas handicap|apuestas handicap asiatico|apuestas handicap baloncesto|apuestas handicap como funciona|apuestas handicap
nba|apuestas handicap nfl|apuestas hipicas online|apuestas hípicas online|apuestas hipicas venezuela|apuestas hockey|apuestas hockey hielo|apuestas hockey patines|apuestas hockey sobre hielo|apuestas holanda argentina|apuestas holanda vs argentina|apuestas hoy|apuestas hoy champions|apuestas hoy futbol|apuestas hoy nba|apuestas hoy pronosticos|apuestas hoy seguras|apuestas impuestos|apuestas inglaterra paises bajos|apuestas inter barca|apuestas inter barcelona|apuestas juego|apuestas juegos|apuestas juegos en linea|apuestas juegos olimpicos|apuestas juegos olímpicos|apuestas juegos olimpicos baloncesto|apuestas juegos online|apuestas juegos virtuales|apuestas jugador sevilla|apuestas jugadores nba|apuestas kings
league americas|apuestas la liga|apuestas la liga española|apuestas la liga hoy|apuestas la liga santander|apuestas las vegas mlb|apuestas las vegas nba|apuestas las vegas nfl|apuestas league of legends mundial|apuestas legal|apuestas legales|apuestas
legales en colombia|apuestas legales en españa|apuestas legales
en estados unidos|apuestas legales españa|apuestas leganes betis|apuestas
libertadores|apuestas licencia|apuestas liga 1 peru|apuestas liga argentina|apuestas liga bbva pronosticos|apuestas liga de campeones|apuestas liga de campeones de baloncesto|apuestas liga de campeones de hockey|apuestas liga españa|apuestas liga española|apuestas
liga santander pronosticos|apuestas ligas de futbol|apuestas
linea|apuestas linea de gol|apuestas liverpool barcelona|apuestas liverpool real
madrid|apuestas lol mundial|apuestas madrid|apuestas madrid arsenal|apuestas madrid atletico|apuestas madrid atletico champions|apuestas madrid barca|apuestas madrid barça|apuestas madrid barca hoy|apuestas
madrid barca supercopa|apuestas madrid barcelona|apuestas madrid barsa|apuestas madrid bayern|apuestas madrid betis|apuestas madrid borussia|apuestas madrid campeon champions|apuestas madrid celta|apuestas
madrid city|apuestas madrid dortmund|apuestas madrid gana la liga|apuestas madrid gana liga|apuestas madrid hoy|apuestas madrid liverpool|apuestas madrid osasuna|apuestas
madrid sevilla|apuestas madrid valencia|apuestas madrid vs arsenal|apuestas madrid vs barcelona|apuestas mallorca osasuna|apuestas mallorca real sociedad|apuestas manchester athletic|apuestas manchester
city real madrid|apuestas mas faciles de ganar|apuestas mas seguras|apuestas mas seguras para
hoy|apuestas masters de golf|apuestas masters de tenis|apuestas maximo goleador eurocopa|apuestas maximo goleador mundial|apuestas mejor jugador eurocopa|apuestas mejores casinos online|apuestas mexico|apuestas méxico|apuestas
mexico polonia|apuestas méxico polonia|apuestas mlb|apuestas mlb hoy|apuestas mlb las vegas|apuestas mlb para
hoy|apuestas mlb pronosticos|apuestas mlb usa|apuestas mma ufc|apuestas momios|apuestas multiples|apuestas múltiples|apuestas multiples como funcionan|apuestas multiples el gordo|apuestas multiples futbol|apuestas mundial|apuestas mundial 2026|apuestas mundial
baloncesto|apuestas mundial balonmano|apuestas
mundial brasil|apuestas mundial campeon|apuestas mundial ciclismo|apuestas mundial clubes|apuestas mundial de baloncesto|apuestas mundial de ciclismo|apuestas
mundial de clubes|apuestas mundial de futbol|apuestas
mundial de fútbol|apuestas mundial de rugby|apuestas mundial f1|apuestas mundial
favoritos|apuestas mundial femenino|apuestas mundial formula 1|apuestas mundial futbol|apuestas mundial
ganador|apuestas mundial lol|apuestas mundial moto gp|apuestas mundial motogp|apuestas mundial
rugby|apuestas mundial sub 17|apuestas mundiales|apuestas mundialistas|apuestas mvp eurocopa|apuestas mvp nba|apuestas mvp nfl|apuestas nacionales de colombia|apuestas nba|apuestas nba all star|apuestas
nba campeon|apuestas nba consejos|apuestas nba esta noche|apuestas nba finals|apuestas nba gratis|apuestas nba
hoy|apuestas nba hoy jugadores|apuestas nba hoy pronosticos|apuestas nba para hoy|apuestas nba playoffs|apuestas nba pronosticos|apuestas nba pronósticos|apuestas nba
pronosticos hoy|apuestas nba tipster|apuestas nfl|apuestas nfl hoy|apuestas nfl las vegas|apuestas
nfl playoffs|apuestas nfl pronosticos|apuestas nfl pronósticos|apuestas nfl semana 4|apuestas nfl super bowl|apuestas nhl|apuestas nhl pronosticos|apuestas octavos eurocopa|apuestas
ofertas|apuestas online|apuestas online argentina|apuestas online argentina legal|apuestas online bono|apuestas online bono bienvenida|apuestas online boxeo|apuestas
online caballos|apuestas online carreras de caballos|apuestas online casino|apuestas
online champions league|apuestas online chile|apuestas online
ciclismo|apuestas online colombia|apuestas online
comparativa|apuestas online con paypal|apuestas online de caballos|apuestas online deportivas|apuestas
online en argentina|apuestas online en peru|apuestas online espana|apuestas online españa|apuestas online esports|apuestas online foro|apuestas online futbol|apuestas online futbol españa|apuestas online golf|apuestas online gratis|apuestas online gratis sin deposito|apuestas online juegos|apuestas online
mexico|apuestas online mma|apuestas online movil|apuestas
online nba|apuestas online net|apuestas online nuevas|apuestas online opiniones|apuestas online paypal|apuestas
online peru|apuestas online seguras|apuestas online sin dinero|apuestas
online sin registro|apuestas online tenis|apuestas online ufc|apuestas online uruguay|apuestas online venezuela|apuestas open britanico golf|apuestas osasuna athletic|apuestas osasuna barcelona|apuestas osasuna real madrid|apuestas
osasuna sevilla|apuestas osasuna valencia|apuestas over|apuestas over 2.5|apuestas over under|apuestas paginas|apuestas pago anticipado|apuestas paises bajos ecuador|apuestas paises bajos inglaterra|apuestas países bajos qatar|apuestas para boxeo|apuestas para champions league|apuestas para el clasico|apuestas para el dia
de hoy|apuestas para el mundial|apuestas para el partido
de hoy|apuestas para eurocopa|apuestas para europa league|apuestas para futbol|apuestas para ganar|apuestas
para ganar dinero|apuestas para ganar dinero facil|apuestas para ganar en la ruleta|apuestas para ganar la champions|apuestas para ganar la eurocopa|apuestas para ganar
la europa league|apuestas para ganar la liga|apuestas para ganar siempre|apuestas para hacer|apuestas para hoy|apuestas para hoy de futbol|apuestas
para hoy europa league|apuestas para hoy futbol|apuestas para juegos|apuestas para la champions league|apuestas para
la copa del rey|apuestas para la eurocopa|apuestas para la europa league|apuestas para la final de la eurocopa|apuestas para la nba hoy|apuestas para los partidos de hoy|apuestas
para partidos de hoy|apuestas para ufc|apuestas partido|apuestas partido aplazado|apuestas partido champions|apuestas partido colombia|apuestas
partido españa marruecos|apuestas partido mundial|apuestas partido suspendido|apuestas partidos|apuestas partidos champions
league|apuestas partidos csgo|apuestas partidos de futbol|apuestas partidos
de futbol hoy|apuestas partidos de hoy|apuestas
partidos eurocopa|apuestas partidos futbol|apuestas partidos hoy|apuestas partidos mundial|apuestas paypal|apuestas peleas de boxeo|apuestas peru|apuestas
perú|apuestas peru brasil|apuestas peru chile|apuestas peru paraguay|apuestas peru uruguay|apuestas peru
vs chile|apuestas peru vs colombia|apuestas pichichi eurocopa|apuestas plataforma|apuestas playoff|apuestas playoff ascenso|apuestas playoff ascenso a primera|apuestas playoff nba|apuestas playoff segunda|apuestas playoff segunda b|apuestas playoffs nba|apuestas playoffs nfl|apuestas polonia argentina|apuestas por argentina|apuestas por internet mexico|apuestas por internet para ganar dinero|apuestas por paypal|apuestas por ronda boxeo|apuestas por sistema|apuestas portugal uruguay|apuestas pre partido|apuestas predicciones|apuestas predicciones futbol|apuestas
primera division|apuestas primera division españa|apuestas promociones|apuestas pronostico|apuestas
pronosticos|apuestas pronosticos deportivos|apuestas pronosticos deportivos tenis|apuestas pronosticos
futbol|apuestas pronosticos gratis|apuestas pronosticos nba|apuestas
pronosticos tenis|apuestas prorroga|apuestas psg barca|apuestas psg barcelona|apuestas puntos por tarjetas|apuestas puntos tarjetas|apuestas que aceptan paypal|apuestas que es handicap|apuestas
que puedes hacer con tu novia|apuestas que siempre ganaras|apuestas que significa|apuestas quien bajara a segunda|apuestas quién bajara a segunda|apuestas quien gana el mundial|apuestas quien gana eurocopa|apuestas quien gana la
champions|apuestas quien gana la eurocopa|apuestas quien gana la
liga|apuestas quien ganara el mundial|apuestas quién ganará el mundial|apuestas quien ganara la champions|apuestas quien ganara la eurocopa|apuestas quien ganara la liga|apuestas rayo barcelona|apuestas real madrid|apuestas
real madrid arsenal|apuestas real madrid athletic|apuestas real madrid atletico|apuestas
real madrid atletico champions|apuestas real madrid atletico
de madrid|apuestas real madrid atlético de madrid|apuestas real madrid
atletico madrid|apuestas real madrid barcelona|apuestas real madrid bayern|apuestas real
madrid betis|apuestas real madrid borussia|apuestas real madrid campeon champions|apuestas real madrid celta|apuestas real madrid champions|apuestas real madrid city|apuestas real madrid girona|apuestas real madrid hoy|apuestas real madrid liverpool|apuestas real madrid manchester city|apuestas
real madrid osasuna|apuestas real madrid real
sociedad|apuestas real madrid valencia|apuestas real madrid villarreal|apuestas real madrid vs arsenal|apuestas real madrid vs atletico|apuestas real madrid vs atlético|apuestas real madrid vs atletico madrid|apuestas real madrid vs barcelona|apuestas real madrid
vs betis|apuestas real madrid vs sevilla|apuestas real madrid vs
valencia|apuestas real sociedad|apuestas real sociedad athletic|apuestas real
sociedad barcelona|apuestas real sociedad betis|apuestas real sociedad psg|apuestas real sociedad real
madrid|apuestas real sociedad valencia|apuestas recomendadas hoy|apuestas regalo de bienvenida|apuestas registro|apuestas resultado exacto|apuestas resultados|apuestas resultados eurocopa|apuestas retirada
tenis|apuestas roma barcelona|apuestas roma sevilla|apuestas
rugby|apuestas rugby mundial|apuestas rugby world cup|apuestas ruleta seguras|apuestas
segunda|apuestas segunda b|apuestas segunda division|apuestas
segunda división|apuestas segunda division b|apuestas
segunda division españa|apuestas seguras|apuestas seguras baloncesto|apuestas seguras calculadora|apuestas seguras en la ruleta|apuestas seguras eurocopa|apuestas seguras foro|apuestas seguras futbol|apuestas
seguras futbol hoy|apuestas seguras gratis|apuestas seguras hoy|apuestas seguras
hoy futbol|apuestas seguras nba|apuestas seguras nba hoy|apuestas seguras
para este fin de semana|apuestas seguras para ganar dinero|apuestas seguras para hoy|apuestas seguras
para hoy fútbol|apuestas seguras para hoy pronósticos|apuestas seguras para mañana|apuestas seguras ruleta|apuestas seguras telegram|apuestas seguras tenis|apuestas semifinales eurocopa|apuestas senegal paises bajos|apuestas
sevilla|apuestas sevilla athletic|apuestas sevilla atletico de
madrid|apuestas sevilla barcelona|apuestas sevilla betis|apuestas sevilla campeon liga|apuestas sevilla celta|apuestas sevilla gana la liga|apuestas sevilla girona|apuestas sevilla inter|apuestas sevilla jugador|apuestas sevilla juventus|apuestas sevilla
leganes|apuestas sevilla madrid|apuestas sevilla manchester united|apuestas sevilla osasuna|apuestas sevilla
real madrid|apuestas sevilla real sociedad|apuestas sevilla roma|apuestas sevilla valencia|apuestas significa|apuestas simples ejemplos|apuestas simples o
combinadas|apuestas sin deposito|apuestas sin deposito inicial|apuestas sin deposito minimo|apuestas sin dinero|apuestas sin dinero real|apuestas sin empate|apuestas sin empate que significa|apuestas sin ingreso minimo|apuestas sin registro|apuestas sistema|apuestas sistema calculadora|apuestas sistema
como funciona|apuestas sistema trixie|apuestas sociedad|apuestas sorteo copa del
rey|apuestas stake|apuestas stake 10|apuestas stake 10 hoy|apuestas super bowl favorito|apuestas super rugby|apuestas supercopa españa|apuestas superliga argentina|apuestas tarjeta roja|apuestas tarjetas|apuestas tarjetas amarillas|apuestas tenis|apuestas tenis atp|apuestas tenis
consejos|apuestas tenis copa davis|apuestas tenis de mesa|apuestas
tenis de mesa pronosticos|apuestas tenis en vivo|apuestas tenis
femenino|apuestas tenis hoy|apuestas tenis itf|apuestas tenis pronosticos|apuestas tenis
pronósticos|apuestas tenis retirada|apuestas tenis roland garros|apuestas tenis seguras|apuestas tenis wimbledon|apuestas tenis wta|apuestas tercera division|apuestas tercera
division españa|apuestas tipos|apuestas tips|apuestas tipster|apuestas tipster para hoy|apuestas topuria holloway cuotas|apuestas torneos de
golf|apuestas torneos de tenis|apuestas trucos|apuestas uefa champions league|apuestas
uefa europa league|apuestas ufc|apuestas
ufc chile|apuestas ufc como funciona|apuestas ufc hoy|apuestas ufc ilia topuria|apuestas ufc online|apuestas ufc pronósticos|apuestas ufc telegram|apuestas ufc topuria|apuestas under over|apuestas unionistas villarreal|apuestas uruguay|apuestas uruguay colombia|apuestas uruguay corea|apuestas uruguay
vs colombia|apuestas us open golf|apuestas us open tenis|apuestas valencia|apuestas valencia barcelona|apuestas valencia betis|apuestas
valencia madrid|apuestas valencia real madrid|apuestas valladolid barcelona|apuestas valladolid valencia|apuestas valor app|apuestas valor
en directo|apuestas valor galgos|apuestas venezuela|apuestas venezuela argentina|apuestas venezuela bolivia|apuestas venezuela ecuador|apuestas villarreal|apuestas villarreal athletic|apuestas
villarreal barcelona|apuestas villarreal bayern|apuestas villarreal betis|apuestas villarreal liverpool|apuestas villarreal manchester|apuestas villarreal manchester united|apuestas villarreal vs real madrid|apuestas
virtuales|apuestas virtuales colombia|apuestas virtuales futbol|apuestas virtuales sin dinero|apuestas vivo|apuestas vuelta a españa|apuestas vuelta españa|apuestas william hill partidos de hoy|apuestas y casino|apuestas y casinos|apuestas y
juegos de azar|apuestas y pronosticos|apuestas y pronosticos de futbol|apuestas
y pronosticos deportivos|apuestas y resultados|apuestas-deportivas|apuestas-deportivas.es pronosticos|arbitro nba apuestas|argentina apuestas|argentina colombia apuestas|argentina croacia apuestas|argentina francia apuestas|argentina mexico apuestas|argentina peru apuestas|argentina uruguay apuestas|argentina vs bolivia apuestas|argentina vs chile apuestas|argentina
vs colombia apuestas|argentina vs francia apuestas|argentina vs.
colombia apuestas|asi se gana en las apuestas deportivas|asiatico apuestas|asiatico en apuestas|asiaticos
apuestas|athletic barcelona apuestas|athletic manchester
united apuestas|athletic osasuna apuestas|athletic
real madrid apuestas|atletico barcelona apuestas|atletico de madrid apuestas|atlético de madrid apuestas|atletico de madrid real madrid apuestas|atletico de madrid
vs barcelona apuestas|atletico madrid real madrid apuestas|atletico madrid vs real madrid apuestas|atletico real madrid
apuestas|atletico vs real madrid apuestas|avisador de
cuotas apuestas|bajada de cuotas apuestas|baloncesto apuestas|barbastro barcelona apuestas|barca apuestas|barca bayern apuestas|barca inter apuestas|barca madrid apuestas|barça madrid
apuestas|barca vs atletico apuestas|barca
vs madrid apuestas|barca vs real madrid apuestas|barcelona – real madrid apuestas|barcelona apuestas|barcelona atletico apuestas|barcelona
atletico de madrid apuestas|barcelona atletico madrid apuestas|barcelona betis apuestas|barcelona casa de apuestas|barcelona inter apuestas|barcelona psg apuestas|barcelona real madrid apuestas|barcelona real sociedad apuestas|barcelona sevilla apuestas|barcelona valencia apuestas|barcelona vs athletic bilbao apuestas|barcelona
vs atlético madrid apuestas|barcelona vs
betis apuestas|barcelona vs celta de vigo
apuestas|barcelona vs espanyol apuestas|barcelona vs girona apuestas|barcelona vs madrid apuestas|barcelona vs real madrid apuestas|barcelona vs real sociedad apuestas|barcelona
vs sevilla apuestas|barcelona vs villarreal apuestas|base de
datos cuotas apuestas deportivas|bayern real madrid apuestas|beisbol apuestas|best america apuestas|bet apuestas chile|bet apuestas en vivo|betis – chelsea apuestas|betis
apuestas|betis barcelona apuestas|betis chelsea apuestas|betis madrid apuestas|betis sevilla apuestas|betsson tu sitio
de apuestas online|blog apuestas baloncesto|blog apuestas ciclismo|blog apuestas nba|blog apuestas tenis|blog
de apuestas de tenis|bono apuestas|bono apuestas deportivas|bono apuestas deportivas sin deposito|bono apuestas gratis|bono apuestas gratis sin deposito|bono apuestas sin deposito|bono bienvenida apuestas|bono bienvenida apuestas deportivas|bono bienvenida apuestas españa|bono bienvenida apuestas sin deposito|bono
bienvenida apuestas sin depósito|bono bienvenida casa apuestas|bono bienvenida casa de apuestas|bono bienvenida marca apuestas|bono casa apuestas|bono casa de
apuestas|bono casa de apuestas sin ingreso|bono casas de apuestas|bono de
apuestas|bono de apuestas gratis sin deposito|bono de bienvenida
apuestas|bono de bienvenida apuestas deportivas|bono de bienvenida casa de apuestas|bono de bienvenida casas de apuestas|bono de casas de
apuestas|bono de registro apuestas|bono de
registro apuestas deportivas|bono de registro casa de apuestas|bono gratis apuestas|bono marca apuestas|bono por registro apuestas|bono por
registro apuestas deportivas|bono por registro casa de apuestas|bono registro apuestas|bono sin deposito apuestas|bono sin depósito apuestas|bono sin deposito apuestas deportivas|bono sin depósito apuestas deportivas|bono sin deposito casa de apuestas|bono sin deposito marca apuestas|bono sin ingreso apuestas|bono
sin ingreso apuestas deportivas|bonos apuestas|bonos
apuestas colombia|bonos apuestas deportivas|bonos apuestas
deportivas sin deposito|bonos apuestas gratis|bonos apuestas sin deposito|bonos apuestas sin depósito|bonos bienvenida apuestas|bonos bienvenida casas apuestas|bonos bienvenida casas de
apuestas|bonos casa de apuestas|bonos casas apuestas|bonos casas de
apuestas|bonos casas de apuestas colombia|bonos casas de apuestas deportivas|bonos casas de apuestas españa|bonos casas de apuestas nuevas|bonos
casas de apuestas sin deposito|bonos casas de apuestas sin depósito|bonos de apuestas|bonos
de apuestas deportivas|bonos de apuestas gratis|bonos de apuestas
sin deposito|bonos de bienvenida apuestas|bonos
de bienvenida apuestas deportivas|bonos de bienvenida
casa de apuestas|bonos de bienvenida casas de apuestas|bonos de bienvenida de casas de apuestas|bonos de bienvenida
en casas de apuestas|bonos de casas de apuestas|bonos de casas de apuestas sin deposito|bonos en casa
de apuestas|bonos en casas de apuestas sin deposito|bonos gratis apuestas|bonos gratis apuestas deportivas|bonos gratis casas de apuestas|bonos gratis sin deposito apuestas|bonos paginas de apuestas|bonos registro casas de
apuestas|bonos sin deposito apuestas|bonos sin depósito apuestas|bonos sin deposito apuestas deportivas|bonos sin deposito casas de apuestas|bot de apuestas deportivas gratis|boxeo apuestas|brasil colombia apuestas|brasil peru apuestas|brasil vs colombia apuestas|buenas apuestas para hoy|buscador cuotas apuestas|buscador de apuestas seguras|buscador de cuotas apuestas|buscador de cuotas de apuestas|buscar apuestas seguras|caballos apuestas|calculador de apuestas|calculador de cuotas apuestas|calculadora apuestas|calculadora apuestas combinadas|calculadora apuestas
de sistema|calculadora apuestas deportivas|calculadora apuestas deportivas seguras|calculadora
apuestas multiples|calculadora apuestas segura|calculadora apuestas seguras|calculadora apuestas sistema|calculadora apuestas
yankee|calculadora arbitraje apuestas|calculadora
cubrir apuestas|calculadora cuotas apuestas|calculadora de apuestas|calculadora de apuestas combinadas|calculadora de apuestas de futbol|calculadora
de apuestas de sistema|calculadora de apuestas deportivas|calculadora de apuestas multiples|calculadora de apuestas seguras|calculadora de apuestas sistema|calculadora de apuestas surebets|calculadora de arbitraje apuestas|calculadora de cuotas apuestas|calculadora de cuotas de apuestas|calculadora para apuestas deportivas|calculadora poisson apuestas|calculadora poisson apuestas deportivas|calculadora poisson para apuestas|calculadora scalping apuestas deportivas|calculadora
sistema apuestas|calculadora stake apuestas|calculadora trading apuestas|calcular apuestas|calcular apuestas deportivas|calcular apuestas futbol|calcular apuestas sistema|calcular cuotas apuestas|calcular cuotas apuestas combinadas|calcular cuotas apuestas deportivas|calcular cuotas de
apuestas|calcular ganancias apuestas deportivas|calcular momios apuestas|calcular probabilidad cuota apuestas|calcular stake apuestas|calcular unidades apuestas|calcular
yield apuestas|calculo de apuestas|calculo de apuestas deportivas|cambio
de cuotas apuestas|campeon champions apuestas|campeon eurocopa apuestas|campeon liga
apuestas|campeon nba apuestas|canales de apuestas gratis|carrera de
caballos apuestas|carrera de caballos apuestas juego|carrera de caballos con apuestas|carrera de galgos apuestas|carreras de caballos apuestas|carreras de caballos
apuestas online|carreras de caballos con apuestas|carreras de
caballos juegos de apuestas|carreras de galgos apuestas|carreras de galgos apuestas
online|carreras de galgos apuestas trucos|carreras galgos apuestas|casa apuestas argentina|casa apuestas atletico
de madrid|casa apuestas barcelona|casa apuestas
betis|casa apuestas bono bienvenida|casa apuestas bono gratis|casa
apuestas bono sin deposito|casa apuestas cerca de mi|casa apuestas chile|casa apuestas colombia|casa apuestas con mejores cuotas|casa apuestas deportivas|casa apuestas españa|casa apuestas española|casa apuestas eurocopa|casa apuestas futbol|casa apuestas mejores
cuotas|casa apuestas mundial|casa apuestas nueva|casa apuestas nuevas|casa apuestas online|casa apuestas peru|casa apuestas
valencia|casa de apuestas|casa de apuestas 10 euros gratis|casa de apuestas argentina|casa de apuestas atletico de madrid|casa de apuestas
baloncesto|casa de apuestas barcelona|casa de apuestas beisbol|casa de apuestas betis|casa de apuestas bono|casa de apuestas bono bienvenida|casa de apuestas bono
de bienvenida|casa de apuestas bono gratis|casa de apuestas bono por registro|casa de apuestas bono sin deposito|casa de apuestas boxeo|casa de apuestas caballos|casa de apuestas carreras
de caballos|casa de apuestas cerca de mi|casa de apuestas cerca
de mí|casa de apuestas champions league|casa de apuestas
chile|casa de apuestas ciclismo|casa de apuestas colombia|casa de apuestas con bono de bienvenida|casa de
apuestas con bono sin deposito|casa de apuestas con cuotas mas altas|casa
de apuestas con esports|casa de apuestas con las mejores cuotas|casa de apuestas con licencia en españa|casa de apuestas
con mejores cuotas|casa de apuestas con pago anticipado|casa de apuestas con paypal|casa de apuestas copa america|casa de apuestas de caballos|casa de apuestas de colombia|casa de apuestas de españa|casa de apuestas de futbol|casa de apuestas de
fútbol|casa de apuestas de futbol peru|casa de apuestas de peru|casa de apuestas
del madrid|casa de apuestas del real madrid|casa
de apuestas deportivas|casa de apuestas deportivas cerca
de mi|casa de apuestas deportivas en argentina|casa de apuestas deportivas en chile|casa de apuestas deportivas en colombia|casa de apuestas deportivas en españa|casa de
apuestas deportivas en madrid|casa de apuestas deportivas españa|casa de apuestas
deportivas españolas|casa de apuestas deportivas madrid|casa de apuestas deportivas mexico|casa de apuestas
deportivas online|casa de apuestas deportivas peru|casa de apuestas deposito 5
euros|casa de apuestas deposito minimo|casa de apuestas deposito minimo 1 euro|casa
de apuestas depósito mínimo 1 euro|casa de apuestas en españa|casa de apuestas en linea|casa de
apuestas en madrid|casa de apuestas en perú|casa de apuestas en vivo|casa de apuestas españa|casa de apuestas
españa inglaterra|casa de apuestas española|casa de apuestas españolas|casa de apuestas esports|casa de
apuestas eurocopa|casa de apuestas europa league|casa de apuestas f1|casa de apuestas formula 1|casa
de apuestas futbol|casa de apuestas ingreso minimo|casa de apuestas ingreso minimo 1 euro|casa de apuestas ingreso mínimo 1 euro|casa de
apuestas legales|casa de apuestas legales en colombia|casa de apuestas legales en españa|casa de apuestas
libertadores|casa de apuestas liga española|casa de apuestas madrid|casa de apuestas mas segura|casa de apuestas mejores|casa de apuestas méxico|casa de
apuestas minimo 5 euros|casa de apuestas mlb|casa de apuestas
mundial|casa de apuestas nba|casa de apuestas nfl|casa de apuestas nueva|casa
de apuestas nuevas|casa de apuestas oficial del real madrid|casa de apuestas oficial real madrid|casa
de apuestas online|casa de apuestas online argentina|casa de apuestas
online chile|casa de apuestas online españa|casa de apuestas online mexico|casa
de apuestas online paraguay|casa de apuestas online peru|casa de apuestas online usa|casa de apuestas online venezuela|casa de apuestas pago anticipado|casa de apuestas
para boxeo|casa de apuestas para ufc|casa de apuestas peru|casa
de apuestas perú|casa de apuestas peru online|casa de apuestas por paypal|casa de apuestas promociones|casa de apuestas que
regalan dinero|casa de apuestas real madrid|casa de apuestas regalo
de bienvenida|casa de apuestas sevilla|casa de apuestas sin dinero|casa
de apuestas sin ingreso minimo|casa de apuestas sin licencia en españa|casa de apuestas sin minimo
de ingreso|casa de apuestas stake|casa de apuestas tenis|casa de apuestas ufc|casa de apuestas
valencia|casa de apuestas venezuela|casa de apuestas virtuales|casa de apuestas vive la suerte|casa oficial de apuestas del real
madrid|casas apuestas asiaticas|casas apuestas bono sin deposito|casas
apuestas bonos sin deposito|casas apuestas caballos|casas apuestas chile|casas apuestas ciclismo|casas apuestas con licencia|casas apuestas con licencia en españa|casas apuestas deportivas|casas apuestas deportivas colombia|casas apuestas deportivas españa|casas apuestas deportivas
españolas|casas apuestas deportivas nuevas|casas apuestas españa|casas apuestas españolas|casas apuestas esports|casas apuestas eurocopa|casas apuestas
golf|casas apuestas ingreso minimo 5 euros|casas apuestas
legales|casas apuestas legales españa|casas apuestas licencia|casas apuestas licencia españa|casas apuestas mexico|casas apuestas mundial|casas apuestas nba|casas apuestas nuevas|casas apuestas nuevas españa|casas
apuestas ofertas|casas apuestas online|casas apuestas paypal|casas apuestas
peru|casas apuestas sin licencia|casas apuestas tenis|casas asiaticas apuestas|casas de apuestas|casas
de apuestas 5 euros|casas de apuestas app|casas de apuestas argentinas|casas de apuestas asiaticas|casas de apuestas baloncesto|casas de apuestas barcelona|casas de apuestas bono bienvenida|casas de apuestas bono de bienvenida|casas de apuestas bono por registro|casas de apuestas bono sin deposito|casas de apuestas bono sin ingreso|casas de apuestas bonos|casas de apuestas bonos de bienvenida|casas de
apuestas bonos gratis|casas de apuestas bonos sin deposito|casas de apuestas boxeo|casas de apuestas caballos|casas de apuestas carreras de caballos|casas de apuestas casino|casas de apuestas casino
online|casas de apuestas cerca de mi|casas de apuestas champions league|casas de apuestas chile|casas de apuestas ciclismo|casas
de apuestas colombia|casas de apuestas com|casas de apuestas
con app|casas de apuestas con apuestas gratis|casas de apuestas con bono|casas de apuestas con bono de
bienvenida|casas de apuestas con bono de registro|casas de apuestas con bono por registro|casas de apuestas con bono sin deposito|casas de apuestas con bonos|casas de apuestas con bonos gratis|casas de
apuestas con bonos sin deposito|casas de apuestas con deposito minimo|casas
de apuestas con esports|casas de apuestas con handicap asiatico|casas
de apuestas con licencia|casas de apuestas
con licencia en españa|casas de apuestas con licencia
españa|casas de apuestas con licencia española|casas de apuestas con mejores cuotas|casas de apuestas con pago anticipado|casas de apuestas con paypal|casas de apuestas con paypal en perú|casas de apuestas con promociones|casas de apuestas con ruleta en vivo|casas de apuestas copa del rey|casas de apuestas de caballos|casas de apuestas de españa|casas de apuestas de futbol|casas de apuestas de fútbol|casas de apuestas de peru|casas de apuestas deportivas|casas de apuestas deportivas asiaticas|casas de apuestas deportivas colombia|casas de apuestas deportivas comparativa|casas
de apuestas deportivas con paypal|casas de apuestas deportivas
en chile|casas de apuestas deportivas en españa|casas de apuestas deportivas en linea|casas de apuestas deportivas en madrid|casas de apuestas
deportivas en mexico|casas de apuestas deportivas en peru|casas de apuestas deportivas en sevilla|casas de apuestas deportivas en valencia|casas de apuestas deportivas españa|casas de apuestas
deportivas españolas|casas de apuestas deportivas legales|casas de apuestas deportivas madrid|casas
de apuestas deportivas mexico|casas de apuestas deportivas nuevas|casas de apuestas deportivas online|casas de apuestas deportivas peru|casas de apuestas deportivas perú|casas
de apuestas deposito minimo 1 euro|casas de apuestas depósito mínimo 1 euro|casas
de apuestas dinero gratis|casas de apuestas en argentina|casas de
apuestas en barcelona|casas de apuestas en chile|casas
de apuestas en colombia|casas de apuestas en españa|casas de apuestas en españa online|casas de
apuestas en linea|casas de apuestas en madrid|casas de apuestas en méxico|casas de
apuestas en peru|casas de apuestas en perú|casas de apuestas en sevilla|casas de apuestas en uruguay|casas de apuestas en valencia|casas de apuestas en venezuela|casas de apuestas equipos de futbol|casas de apuestas españa|casas de
apuestas españa alemania|casas de apuestas españa inglaterra|casas de apuestas españa licencia|casas de apuestas españa nuevas|casas de apuestas españa online|casas de apuestas española|casas de apuestas españolas|casas de apuestas españolas
con licencia|casas de apuestas españolas online|casas de apuestas esports|casas de apuestas
eurocopa|casas de apuestas eurocopa 2024|casas de apuestas europa league|casas de apuestas f1|casas de
apuestas fisicas en barcelona|casas de apuestas fisicas en españa|casas de apuestas
formula 1|casas de apuestas fuera de españa|casas de apuestas futbol|casas de apuestas fútbol|casas de apuestas
futbol españa|casas de apuestas ganador eurocopa|casas de apuestas gratis|casas de apuestas ingreso
minimo|casas de apuestas ingreso minimo 1 euro|casas de apuestas ingreso minimo
5 euros|casas de apuestas inter barcelona|casas de apuestas legales|casas de apuestas legales en colombia|casas de apuestas legales
en españa|casas de apuestas legales en mexico|casas de apuestas legales
españa|casas de apuestas legales mx|casas de apuestas licencia|casas de apuestas licencia españa|casas de apuestas lista|casas de apuestas madrid|casas de
apuestas mas seguras|casas de apuestas mejores bonos|casas de
apuestas mejores cuotas|casas de apuestas mexico|casas de apuestas méxico|casas de apuestas minimo 5 euros|casas
de apuestas mlb|casas de apuestas mundial|casas de apuestas mundial
baloncesto|casas de apuestas mundiales|casas de apuestas nba|casas de apuestas no reguladas
en españa|casas de apuestas nueva ley|casas de apuestas nuevas|casas de
apuestas nuevas en colombia|casas de apuestas nuevas en españa|casas de apuestas nuevas españa|casas de apuestas ofertas|casas de apuestas online|casas de
apuestas online argentina|casas de apuestas online colombia|casas de apuestas online deportivas|casas
de apuestas online ecuador|casas de apuestas online en argentina|casas de apuestas online en chile|casas de apuestas online en colombia|casas de apuestas online en españa|casas de apuestas
online en mexico|casas de apuestas online españa|casas de apuestas online mas fiables|casas de apuestas online mexico|casas de apuestas online nuevas|casas de apuestas
online peru|casas de apuestas online usa|casas de apuestas
online venezuela|casas de apuestas pago paypal|casas de
apuestas para ufc|casas de apuestas paypal|casas de apuestas peru
bono sin deposito|casas de apuestas presenciales en españa|casas de apuestas promociones|casas de apuestas que
QQ887P.COM LÀ THƯƠNG HIỆU CÁ CƯỢC UY TÍN CỦA NHÀ CÁI QQ88. mang đến casino, bắn cá, nổ hũ, đá gà…
QQ88 mang đến sân chơi giải trí an toàn, minh bạch cùng hệ thống ưu đãi hấp dẫn mỗi ngày. Hỗ trợ 24/7, đăng ký nhanh gọn, đồng hành lâu dài cùng cược thủ.
Риск от наркотиков — этто сложная хоботня, обхватывающая физиологическое, психическое и соц состояние здоровья человека.
Употребление таковских
наркотиков, как кокаин, мефедрон, ямба, «наркотик» чи «бошки»,
что ль огласить буква неконвертируемым результатам как для организма, яко равным
образом чтобы общества в течение целом.
Но хоть при развитии подневольности возможно электровосстановление — ядро, чтоб зависимый явантроп направился
согласен помощью. Важно запоминать, яко наркомания врачуется, а также оправдание бабахает шанс сверху новейшую жизнь.
QQ88 media LÀ Trang chủ CÁ CƯỢC UY TÍN CỦA NHÀ CÁI QQ88. mang đến casino, bắn cá, nổ hũ, đá gà…
What a data of un-ambiguity and preserveness of precious know-how
on the topic of unpredicted feelings.
QQ88 là nhà cái trực tuyến chuyên cung cấp các sản phẩm cá cược đa dạng như Thể Thao, Casino Live, Nổ Hũ, Bắn Cá, Đá Gà và Xổ Số trực tuyến. Nền tảng được đầu tư công nghệ hiện đại, tối ưu tốc độ truy cập và bảo mật thông tin người chơi, mang đến trải nghiệm giải trí ổn định trên cả PC lẫn Mobile.
QQ88 là nhà cái cá cược trực tuyến cung cấp hệ sinh thái giải trí toàn diện gồm Cá cược Thể Thao, Casino Live, Slot Game (Nổ Hũ), Bắn Cá, Đá Gà và Xổ Số online.
There is certainly a lot to learn about this issue. I
really like all of the points you made.